This year’s flu season is not messing around.

As the virus has swept the US in recent months, people have turned to some strange habits to keep illness at bay, like chugging orange juice, “starving” their fevers, and taking antibiotics. (Spoiler: None of these will help.)
Orange juice is high in sugar and there’s little to no evidence that the vitamin C it contains helps beat viruses.
Depriving yourself of nutrients while you’re sick may also backfire; your weakened immune system needs nutrients to fight off illness. And antibiotics kill bacteria, not viruses – which characterise both the flu and the common cold.
Instead, there are several research-backed steps you can take to fight off illness.
Keep in mind, too, that the symptoms of the flu and the common cold can be very similar, but these preventive and defensive tips should help in most cases.
1. Gargle with plain water
If you’re just starting to feel a cold coming on, try gargling with plain water. A study of close to 400 healthy volunteers published in the American Journal of Preventive Medicine found that those who gargled with plain water were significantly less likely to come down with upper-respiratory-tract infections (URTIs) – a type of infection often linked with colds and the flu – during the study period.
The researchers concluded that “simple water gargling was effective to prevent URTIs among healthy people.”
2. Have some chicken soup
Strangely enough, several recent studies have suggested that chicken soup may actually reduce the symptoms of a cold.
The jury’s still out on precisely why this old-school remedy appears to help, but the available evidence suggests that some component of the soup helps calm down the inflammation that triggers many cold symptoms.
For a study published in the journal Chest, the official publication of the American College of Chest Physicians, researchers found that chicken soup appeared to slow the movement of neutrophils, the white blood cells that are the hallmark of acute infection.
In an attempt to decipher precisely which part of the soup was beneficial, they also tested some of the components individually, and concluded that both the vegetables and the chicken appeared to have “inhibitory activity”.
3. Get plenty of rest
Getting enough sleep – somewhere between seven and nine hours a night – is key to a properly functioning immune system, which plays a critical role in both helping fight off an existing cold and defending you against a new one.
For a 2009 study published in JAMA Internal Medicine, researchers tracked the sleep habits of 153 healthy men and women for two weeks to get a sense of their sleep patterns.
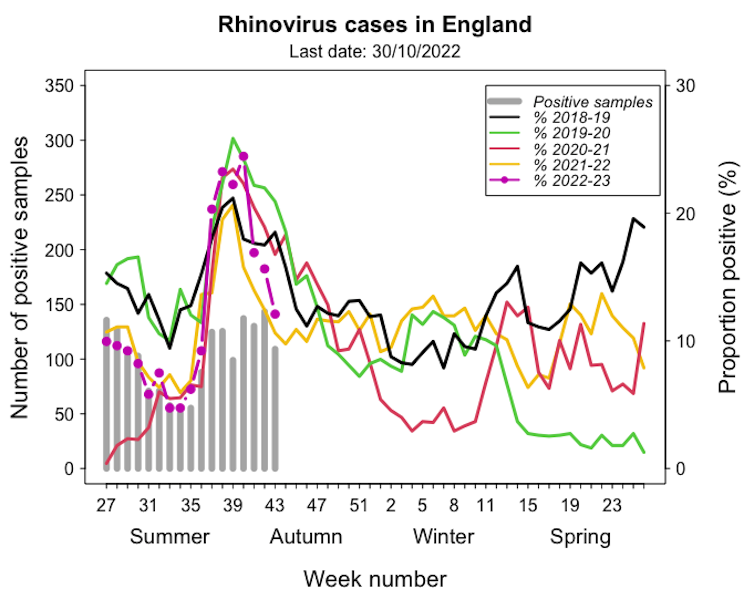
Then, they gave them nasal drops containing rhinovirus, also known as the common cold, and monitored them for five more days.
Volunteers who regularly got less than seven hours of sleep were nearly three times more likely to come down with the cold than those who slept eight hours or more each night.
4. Try a zinc supplement or lozenge
Unlike vitamin C, which studies have found likely does nothing to prevent or treat the common cold, zinc may actually be worth a shot this season.
The mineral seems to interfere with the replication of rhinoviruses, the bugs that cause the common cold.
In a 2011 review of studies of people who’d recently gotten sick, researchers looked at those who’d started taking zinc and compared them with those who just took a placebo. The ones on zinc had shorter colds and less severe symptoms.
Zinc is a trace element that the cells of our immune system rely on to function. Not getting enough zinc (Harvard Medical School researchers recommend 15-25 mg of zinc per day) can affect the functioning of our T-cells and other immune cells.
But it’s also important not to get too much: an excess of the supplement may actually interfere with the immune system’s functioning and have the opposite of the intended result.
5. For aches and pains, acetaminophen (Tylenol) or (Advil) may help
Over-the-counter pain medications like Advil and Tylenol can help with the aches and pains that often accompany colds and the flu. The research on which one provides superior relief for viruses is inconclusive, however.
A 2013 study published in the British Medical Journal that looked at close to 1,000 people with upper-respiratory infections (not colds) suggested that Tylenol provided stronger relief, but it’s important to keep in mind that because Advil is an anti-inflammatory, it may be better for soothing swollen glands.
6. Use honey to soothe a cough
If you hate the taste of cough syrup, you’re in luck: The WHO actually recommends honey as a cough medication for children.
A 2012 Pediatrics study of 300 children who’d been sick for a week or less found that those who were given 10 grams of honey at bedtime had fewer cough symptoms (compared with those who were given a placebo).
Oddly enough, the kids given honey also slept more soundly.
7. If your nasal passages are blocked, try a decongestant and skip the Vicks.
According to Jay L. Hoecker, an emeritus member of the department of pediatric and adolescent medicine at the Mayo Clinic, menthol rubs like Vicks VapoRub won’t help relieve a stuffy nose.
Instead, the “strong menthol odor of VapoRub tricks your brain, so you feel like you’re breathing through an unclogged nose,” he wrote in a recent post for the Clinic.
What he recommends for congestion are over-the-counter decongestant tablets like Sudafed and nasal sprays, which studies suggest may narrow the blood vessels in the lining of your nose and help reduce swelling.
8. If your stomach is also upset, ginger can provide some relief.
Sometimes, getting a cold seems to throw our whole body out of whack. If you’re also feeling nauseated, bloated, or experiencing indigestion, ginger may help.
A study published in the British Journal of Anesthesia comparing people taking a placebo with those taking ginger found that just one gram of the root was helpful in alleviating symptoms of seasickness, morning sickness, and nausea induced by chemotherapy.
Ginger may also be helpful for relieving gas and indigestion in general, Stephen Hanauer, a professor of gastroenterology at Northwestern University’s Feinberg School of Medicine, told Prevention.
The root speeds up stomach emptying and helps release gas, Hanauer said.