‘Ablation is often safer for patients that have lesions in the no-fly zones’
Never let it be said that lung cancer patients don’t present clinicians with a unique set of circumstances. For instance, many primary lung cancer patients have “multiple medical comorbidities, often have a heavy smoking history, and a lot of cardiovascular disease — and this restricts the therapeutic options that are available to them,” noted Alice Gillams, MB ChB, from The London Clinic.
Then there are those with secondary metastases in the lungs: “These patients are often more physically fit than the primary lung cancer patients, but they have multiple sites of disease, which automatically puts them at stage IV,” she observed in a Cardiovascular and Interventional Radiological Society of Europe (CIRSE) interview at the 2016 European Conference on Interventional Oncology (ECIO) in Dublin.
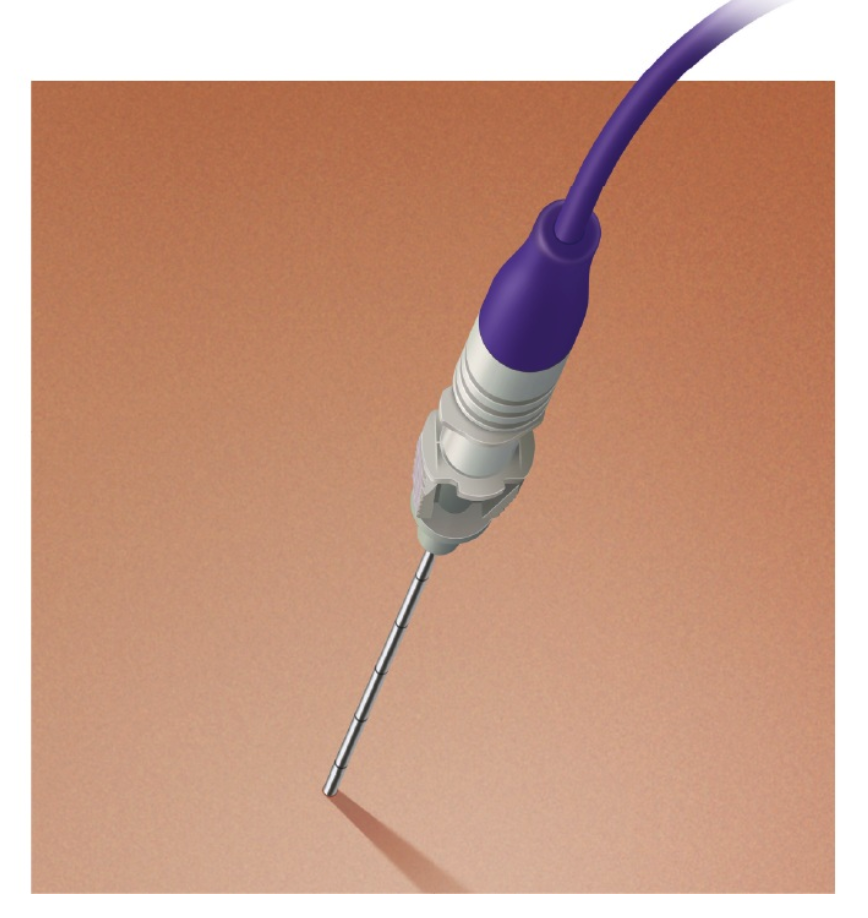
Fortunately, ablation therapy — delivered via radiofrequency ablation (RFA), microwave ablation (MWA), interstitial laser ablation (ILA), irreversible electroporation (IRE), or cryoablation — has demonstrated good efficacy for this patient cohort.
The benefit of percutaneous thermal ablation is that it has very little impact on lung function, a low complication rate, a limited hospital stay for patients, and can be repeated multiple times, Gillams said. “These patients don’t get just one metastases — they get another metastases sometime later, and another, and another. Having a reiterative therapy that effectively eradicates each metastases is a real breakthrough for ablation.”
However, each ablation modality comes with its own benefits and drawbacks. “For example, with cryoablation you seem to get less pneumothoraces, but you get a little bit more bleeding. So, you choose the ablation technology dependent on the patient — where their tumors are, how big the tumors are, whether they can undergo general anesthesia, what their comorbidities are, and so on.”
International researchers are doing their part to advance the use of ablation therapy for secondary metastases in the lungs.
Ablation Options
In a review article, Han Qi, MD, and Weijun Fan, MD, from the Sun Yat-sen University Cancer Center in Guadngdong Sheng, China, highlighted the results of current and previous ablation treatments for lung metastases with a focus on the value of ablation therapy for different kinds of lung metastases.
“The lungs are the second most prominent metastatic organs, after the liver, in which malignant tumors develop,” they wrote. “Lung metastasis often occurs through the following routes: hematogenous spread, lymphatic spread, direct infiltration or overspread, and airway transcoelomic spread.”
Colorectal cancer patients are particularly prone to developing lung metastases, with 10% to 20% of patients progressing this way. In this patient population, the median survival duration of RFA combined with systemic chemotherapy was 44.2 versus 24.7 months for systemic chemotherapy alone. The 3-year survival rates were 87.5% versus 33.3% (P=0.0041).
Bone and soft tissue sarcoma patients are another population that show a propensity for distant metastases (10-15% of osteosarcoma cases; 20% of soft tissue sarcoma cases), with about 85% of those locating in the lung, the authors noted.
In small-sample populations, ablation has demonstrated 1-year and 3-year survival rates comparable to those of resection (90-92% at 1 year; 60-85% at 3 years). For elderly patients and those who require controlling tumor recurrence, ablation may be the preferred therapy, Qi and Fan said.
Renal cancer often presents (25-30% of cases) with distant metastases at the time of diagnosis, with the lung the most common site. Ablation therapy has shown a 5-year survival rate of 53.8%, compared with approximately 40% in surgical resection with this patient group.
A major difficulty for traditional therapies with this cohort is the extent of metastasis, which trends toward very high, the authors pointed out.
Primary liver cancer is also associated with a high incidence of secondary lung metastases, with 20% or greater being common. If the primary lesion is well controlled, RFA for secondary lung tumors can be beneficial to patients who cannot tolerate surgery. Survival rates in this cohort range from 73% to 83% at year 1 and 30% to 57% at year 3.
Nasopharyngeal cancer also kicks out distant metastases, with the lung among the more prevalent areas of occurrence. Small studies evaluating ablation with MWA and RFA among this group found the therapy to be effective.
In one study, only five of 27 patients presented with new lung metastases 1 year after complete MWA ablation of their lung tumors, Qi and Fan explained. In another group, the median survival of nasopharyngeal cancer patients with secondary lung metastases treated with RFA combined with chemotherapy was significantly longer than for those who received only chemotherapy (77.1 versus 32.4 months, P=0.009).
Percutaneous Lung Ablation Therapy
David Morris, MD, from St. George Hospital in Sydney, New South Wales, and colleagues, tracked the survival of 21 colorectal cancer patients with secondary lung metastases (average of three lesions, 13 patients with bilobar disease) who underwent percutaneous lung ablation therapy (PLAT), either with RFA or MWA.
The overall survival (OS) post lung metastases was 18 months or more in the patients who had ablation therapy compared with those who had systemic chemotherapy (26 versus 14 months, P =0.03). However, 38% of the group had local tumor recurrence post-ablation.
A peritoneal carcinomatosis index >10 (hazard ratio 3.48, 95% CI 1.69-7.19), presence of liver metastases (HR 2.49, 95% CI 1.24-5.03), and ablation (HR 0.43, 95% CI 0.20-0.93) were identified as significant predictors of OS following a diagnosis of pulmonary metastases in colorectal cancer patients.
The Chinese and Australian authors noted that patient sample sizes can be problematic for lung cancer ablation studies.
“Trials have been quite difficult to organize because the randomization process has been so tricky,” Gillams commented. “I think what we’re doing at the moment is gathering more experience, larger data databases, more complete data, more uniform patient populations, and extrapolating retrospective data as to where we should go forward in terms of numbers.”
CT-Guided RFA
Xin-Min Li, MD, from the 306th Hospital of the People’s Liberation Army in Beijing, and colleagues, put together one of the larger retrospective studies (476 consecutive patients) of CT-guided lung tumor RFA, although the data is from a single institution.
The group reviewed the records of 668 neoplasms treated in 476 medically inoperable patients (294 men, 60 women; median age of 74; range 29–84) who underwent CT-guided RFA during a 12-year period (2004-2016) at their facility.
Each patient had clinical or pathologic evidence of a neoplastic lesion. The researchers found that 22.1% of the patients presented with primary non–small cell lung cancer (NSCLC), 22.3% had recurrent NSCLC, 45.2% were treated for secondary metastases, and 10.3% had treatment for small cell lung cancer (SCLC).
The medical records revealed a mean lesion size of 3.8 cm (range of 1–16 cm), and that 21 lesions were re-treated from one to four times. All procedures were technically successful, and there were no procedure-related deaths. A total of 21.8% of the cases had low-grade fever.
The probabilities for various OS rates for primary NSCLC, metastases, recurrence, and small-cell lung cancer (SCLC), respectively, were as follows:
- 1 year: 98.1%, 59.7%, 93.3%, 89.4%
- 2 year: 86.6%, 18.5%, 59.1%, 67.5%
- 3 year: 68.9%, 8%, 49.6%, 39.1%
- 5 year: 34.5%, 3.4%, 19.7%, 16.5%
- 10 year: 9.5%, 1.5%, 0%, 0%
In primary NSCLC, progression-free survival and OS were significantly related to tumor size, but there was no significant difference in recurrent NSCLC, metastasis, and peripheral SCLC.
“RFA offers good local control of recurrent NSCLC, lung metastases, and SCLC,” the researchers stated.
Peter Kennedy, MD, from Royal Victoria Hospital in Belfast, Ireland, concurred, noting that interventional oncology is the service that surgical and radiotherapy colleagues turn to when they’re stuck on treatment options for their cancer patients: “In terms of surgery, these are patients that are not surgically fit — per lung function tests, per cardiac history, per other co-morbidities,” he said in another CIRSE video interview at ECIO.
“Ablation is often safer for patients that have lesions in the no-fly zones or have pulmonary fibrosis or have synchronous bi-lateral tumors — these are the typical patients that I’m seeing.”