The human brain is profoundly complex, consisting of tens of billions of neurons that form trillions of interconnections. This complex neural wiring that allows us to think, feel, move, and act is surrounded by what’s called the blood-brain barrier (BBB), a dense sheet of cells and blood vessels. The BBB blocks dangerous toxins and infectious agents from entering the brain, while allowing nutrients and other essential small molecules to pass right through.
This gatekeeping function helps to keep the brain healthy, but not when the barrier prevents potentially life-saving drugs from reaching aggressive, inoperable brain tumors. Now, an NIH-funded team reporting in the journal Nature Materials describes a promising new way to ferry cancer drugs across the BBB and reach the sites of disease [1]. While the researchers have not yet tried this new approach in people, they have some encouraging evidence from studies in mouse models of medulloblastoma, an aggressive brain cancer that’s diagnosed in hundreds of children each year.
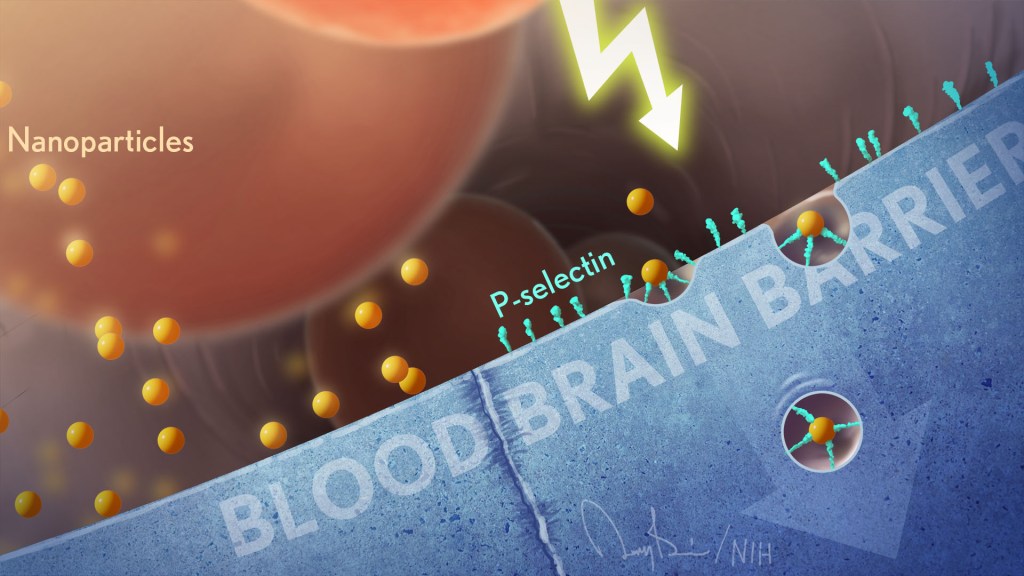
The team, including Daniel Heller, Memorial Sloan Kettering Cancer Center, New York, NY, and Praveen Raju, Icahn School of Medicine at Mount Sinai, New York, NY, wanted to target a protein called P-selectin. The protein is found on blood vessel cells at sites of infection, injury, or inflammation, including cancers. The immune system uses such proteins to direct immune cells to the places where they are needed, allowing them to exit the bloodstream and enter other tissues.
Heller’s team thought they could take advantage of P-selectin and its molecular homing properties as a potential way to deliver cancer drugs to patients. But first they needed to package the drugs in particles tiny enough to stick to P-selectin like an immune cell.
That’s when they turned to a drug-delivery construct called a nanoparticle, which can have diameters a thousand times smaller than that of a human hair. But what’s pretty unique here is the nanoparticles are made from chains of sugar molecules called fucoidan, which are readily extracted from a type of brown seaweed that grows in Japan. It turns out that this unlikely ingredient has a special ability to attract P-selectin.
In the new study, the researchers decided to put their novel fucoidan nanoparticles to the test in the brain, while building on their previous animal work in the lungs [2]. That work showed that when fucoidan nanoparticles bind to P-selectin, they trigger a process that shuttles them across blood vessel walls.
This natural mechanism should also allow nanoparticle-packaged substances in the bloodstream to pass through vessel walls in the BBB and into the surrounding brain tissue. The hope was it would do so without damaging the BBB, a critical step for improving the treatment of brain tumors.
In studies with mouse models of medulloblastoma, the team loaded the nanoparticles with a cancer drug called vismodegib. This drug is approved for certain skin cancers and has been tested for medulloblastoma. The trouble is that the drug on its own comes with significant side effects in children at doses needed to effectively treat this brain cancer.
The researchers found that the vismodegib-loaded nanoparticles circulating in the mice could indeed pass through the intact BBB and into the brain. They further found that the particles accumulated at the site of the medulloblastoma tumors, where P-selectin was most abundant, and not in other healthy parts of the brain. In the mice, the approach allowed the vismodegib treatment to work better against the cancer and at lower doses with fewer side effects.
This raised another possibility. Radiation is a standard therapy for children and adults with brain tumors. The researcher found that radiation boosts P-selectin levels specifically in tumors. The finding suggests that radiation targeting specific parts of the brain prior to nanoparticle treatment could make it even more effective. It also may help to further limit the amount of cancer-fighting drug that reaches healthy brain cells and other parts of the body.
The fucoidan nanoparticles could, in theory, deliver many different drugs to the brain. The researchers note their promise for treating brain tumors of all types, including those that spread to the brain from other parts of the body. While much more work is needed, these seaweed-based nanoparticles may also help in delivering drugs to a wide range of other brain conditions, such as multiple sclerosis, stroke, and focal epilepsy, in which seizures arise from a specific part of the brain. It’s a discovery that brings new meaning to the familiar adage that good things come in small packages.
