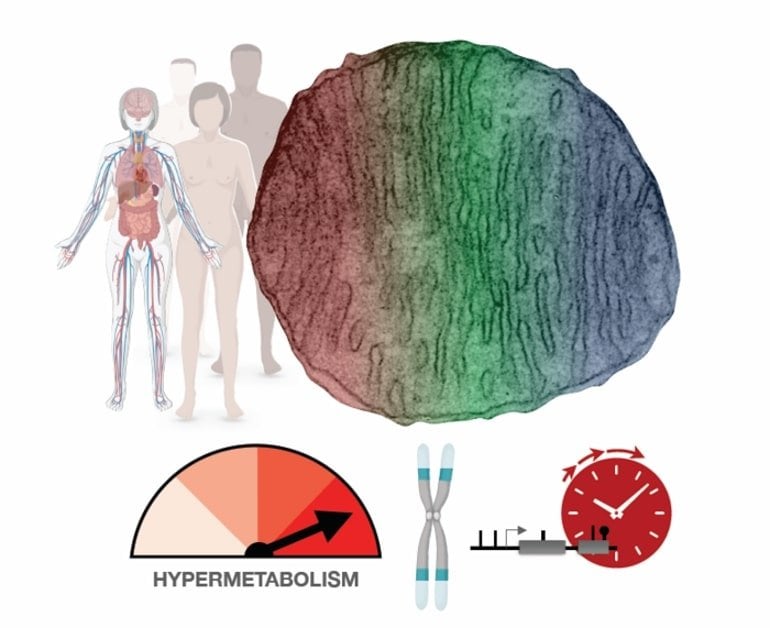
Summary: Human cells with impaired mitochondria expend more energy. While this hypermetabolism enhances a cell’s short-term survival, it also dramatically increases the rate at which the cell ages.
Source: Columbia University
Why do cells, and by extension humans, age? The answer may have a lot to do with mitochondria, the organelles that supply cells with energy. Though that idea is not new, direct evidence in human cells had been lacking. Until now.
In a study published Jan. 12 in Communications Biology, a team led by Columbia University researchers has discovered that human cells with impaired mitochondria respond by kicking into higher gear and expending more energy.
While this adaptation—called hypermetabolism—enhances the cells’ short-term survival, it comes at a high cost: a dramatic increase in the rate at which the cells age.
“The findings were made in cells from patients with rare mitochondrial diseases, yet they may also have relevance for other conditions that affect mitochondria, including neurodegenerative diseases, inflammatory conditions, and infections,” says principal investigator Martin Picard, PhD, associate professor of behavioral medicine (in psychiatry and neurology) at Columbia University Vagelos College of Physicians and Surgeons.
“In addition, hypermetabolism may be a key reason why most cells deteriorate as we get older.”
Hypermetabolic cells age faster
It was generally assumed that mitochondrial defects (which impair the conversion of food sources into usable energy) would force cells to slow their metabolic rate in an effort to conserve energy.
However, by analyzing metabolic activity and energy consumption in cells from patients with mitochondrial diseases, the researchers found that cells with impaired mitochondria double their energy expenditure.
Moreover, re-analyzing data from hundreds of patients with different mitochondrial diseases showed that mitochondrial defects also increase the energetic cost of living at the whole-body level.
Although this energy boost keeps cells running, it also degrades the cell’s telomeres (caps that protect the ends of our chromosomes) and activates stress responses and inflammation. The net effect accelerates biological aging.
“When cells expend more energy to make proteins and other substances essential for short-term survival, they’re likely stealing resources from processes that ensure long-term survival, like maintaining telomeres,” says Gabriel Sturm, a graduate student and lead author on this study.
Hypermetabolism, fatigue, and aging
This hypermetabolic state could explain why people with mitochondrial diseases experience fatigue and exercise intolerance, among other symptoms.
“To make up for the extra energy use in your cells, your body ‘tells’ you not to overexert yourself, to conserve energy. We likely see the same dynamic as people age and their vitality diminishes,” Picard says.
The study doesn’t point to any new remedies for patients with mitochondrial diseases, which are currently not treatable, but it does reinforce the current recommendations for patients to move more.
“That may seem counterintuitive, since if you’re more active, you’re going to expend more energy and possibly make your symptoms worse,” Sturm says.
“But exercise is known to increase the efficiency of an organism. An individual who runs, for example, uses less energy to sustain basic bodily processes than someone who is not physically active.”
Improving organismal efficiency, which would lower energy use in the cells and improve fatigue and other symptoms, may partially explain the health benefits of exercise in patients with mitochondrial diseases and otherwise healthy people.
In their search for new treatments for mitochondrial diseases, researchers should focus on hypermetabolism, Picard says. “Although mitochondrial defects do impair the ability of cells to produce energy, energy deficiency may not be the primary disease initiator. Our study shows these defects increase energy consumption. To move the needle therapeutically, we may need to target hypermetabolism. We need more research to know if that would work.”
Hypermetabolism is also common to other diseases. If increased cellular energy expenditure plays a causal role in driving the aging process, targeting hypermetabolism may be a way to improve fatigue, improve people’s quality of life, or even to slow biological aging.
Abstract
OxPhos defects cause hypermetabolism and reduce lifespan in cells and in patients with mitochondrial diseases
Patients with primary mitochondrial oxidative phosphorylation (OxPhos) defects present with fatigue and multi-system disorders, are often lean, and die prematurely, but the mechanistic basis for this clinical picture remains unclear.
By integrating data from 17 cohorts of patients with mitochondrial diseases (n = 690) we find evidence that these disorders increase resting energy expenditure, a state termed hypermetabolism.
We examine this phenomenon longitudinally in patient-derived fibroblasts from multiple donors. Genetically or pharmacologically disrupting OxPhos approximately doubles cellular energy expenditure.
This cell-autonomous state of hypermetabolism occurs despite near-normal OxPhos coupling efficiency, excluding uncoupling as a general mechanism. Instead, hypermetabolism is associated with mitochondrial DNA instability, activation of the integrated stress response (ISR), and increased extracellular secretion of age-related cytokines and metabokines including GDF15.
In parallel, OxPhos defects accelerate telomere erosion and epigenetic aging per cell division, consistent with evidence that excess energy expenditure accelerates biological aging.
To explore potential mechanisms for these effects, we generate a longitudinal RNASeq and DNA methylation resource dataset, which reveals conserved, energetically demanding, genome-wide recalibrations.
Taken together, these findings highlight the need to understand how OxPhos defects influence the energetic cost of living, and the link between hypermetabolism and aging in cells and patients with mitochondrial diseases.

