By Dr. Mercola
Osteoporosis is a common problem, affecting an estimated 1 in 10 women worldwide at the age of 60.1 By the time a woman reaches the age of 80, she has a 2-in-5 chance of developing osteoporosis. In most people, sometime during your 30s your bone mass will start to gradually decline. For women, that bone loss can significantly speed up during the first decade of menopause.
Statistics suggest that, worldwide, 1 in 3 women and 1 in 5 men over the age of 50 will experience an osteoporosis-related bone fracture. In 2000, there were 9 million osteoporotic fractures, including 1.6 million hip fractures — a quarter of which occurred in men — which can lead to a significant decline in health and quality of life. Hip fractures can also be life-threatening. Twenty percent of those who break a hip die in the first 12 months following the fracture.
Statistics also reveal that osteoporosis is becoming more prevalent. In the decade between 1990 and 2000, the number of hip fractures increased by 25 percent worldwide.2 So, what can be done about this problem? It’s important to realize that osteoporosis is preventable by “proper living,” meaning eating right, getting nutritional movement and effective exercise.
Weight-bearing exercises are particularly important for the prevention of osteoporosis, which is characterized by porous and fragile bones. Unfortunately, drugs are typically the first-line remedy recommended by conventional doctors. This is tragic, considering these drugs do more harm than good.
The Case Against Osteoporosis Drugs
For example, oral bisphosphonate osteoporosis drugs such as Actonel, Boniva and Fosamax, are associated with a two-fold increased risk of esophageal cancer.3 Research also shows that, over time, these kinds of drugs will actually worsen your condition, because all you’re doing is fooling your body into producing denser but weaker bone.
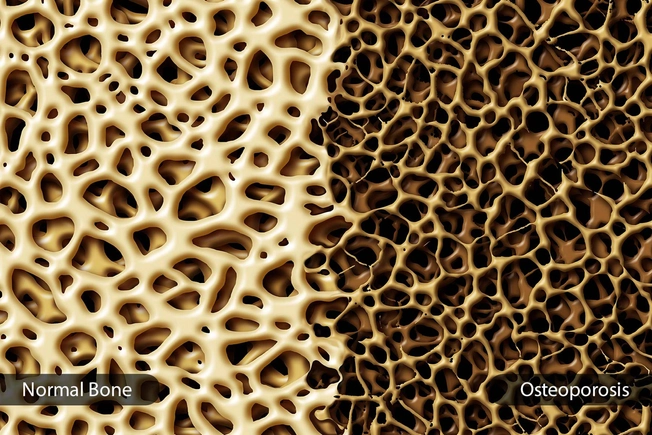
This may sound like an oxymoron, but here’s how it works: Healthy bones maintain strength from a continual process of bone breakdown and bone rebuilding. Osteoclasts are cells that break down bone; osteoblasts are the cells that rebuild it. Healthy bone undergoes a dynamic process of cyclical removal of unhealthy bone and replacement with new bone. This is how they remain strong.
In osteoporosis, the net rate of bone resorption (breakdown) exceeds the rate of bone formation, which results in a decrease in bone mass. Bisphosphonates and similar drugs do not actually help your body build new bone. These drugs work by killing off your osteoclasts, which halts the normal bone repair process since you now lack the cells that break bone down.
The end result is increased bone density, but denser bone is not stronger! Eventually your bones become weaker and more prone to fracture. In women who have been taking a bisphosphonate-type drug for five or more years, their bones have literally lost the ability to regenerate and this is why many are still faced with more brittle bones and fractures.
Your Lifestyle Largely Determines Your Osteoporosis Risk
While diet certainly plays an important role, weight-bearing exercise is one of the most effective remedies against osteoporosis.4 For example, the walking lunge is a great exercise for building bone density in your hips, even without any additional weights. It is an absolutely extraordinary exercise and doesn’t cost anything to do. You can use YouTube to find demonstrations of how to do it properly.
Balance-building exercises like yoga and Tai Chi are also recommended. As long as you have strong muscles, bones and steady balance, your risk of falling is minimized. Should you fall, your chances of actually breaking a bone are also dramatically reduced.
Needless to say, the earlier you start exercising, the better — provided you keep it up. Exercise is really a lifelong lifestyle component, not a temporary fix for any particular problem. That said, even if you’re older, you can still improve your bone health. It’s never too late to start exercising. It just gets a bit more challenging, since you’re starting at a lower level of fitness with each passing year of inactivity. Below I’ll offer some effective exercise alternatives that can be particularly helpful if your fitness level is low. As noted by Fight Aging:5
“The research materials … argue that the majority of people are not aware of the degree to which they are harming themselves, and that efforts should be taken to correct this … In our technological society of cheap calories, easy transportation, and replacements for physical labor, most people eat too much and exercise too little.
That becomes ever more pronounced over the years … This has a cost when it comes to health … Avoidable damage done to health over the long term is often referred to as secondary aging. It includes … accelerated loss of muscle resulting from lack of exercise. Near everyone in later life fails to exercise sufficiently, as demonstrated by study after study showing improvement in the muscle and health of even very old people following modest resistance exercise programs.”
Exercise Naturally Builds Stronger Bones
Aside from walking lunges, high-impact exercises such as sprinting and jumping are also effective, as is weight training.6,7 In one 2014 study,8 women between the ages of 25 and 50 who performed a minimum of 10 “flea leaps” in a row, twice a day for four months, significantly increased the bone density in their hipbones.
An earlier study9 found hopping and weightlifting increased bone density in the spine by 2 percent. Weight training targeting both the upper body and legs was particularly effective. Keep in mind that you’re not restricted to any particular type of exercise though. For example, you don’t have to use weight gym equipment if you don’t want to. Other examples of high-impact weight-bearing exercises recommended by the U.S. National Osteoporosis Foundation include:10
- Dancing
- High-impact aerobics
- Hiking
- Jumping rope
- Climbing stairs
- Playing tennis
Lower impact weight-bearing exercises, which are a safer alternative if you’re frail include:
- Low-impact aerobics
- Stair-step machines
- Fast walking
Similarly, in lieu of weights, you can use just your body weight, elastic exercise bands or functional movements such as raising and lowering your body onto your tippy toes. Three other exercise alternatives worth mentioning that can be particularly helpful if you’re severely obese, old and frail, recovering from an injury or otherwise struggle with mobility, balance and low fitness are Whole Body Vibrational Training (WBVT), blood restriction training and the nitric oxide (NO) dump.
Whole Body Vibrational Training — An Excellent Choice for the Elderly
WBVT using a Power Plate is a safe, natural way to improve bone strength and density, thereby warding off osteoporosis. Best of all, it’s gentle enough even for the disabled and elderly, who may not be able to engage in exercises like leaping, hopping, sprinting or weightlifting.
In one six-month-long study,11 WBVT was found to produce a significant increase in hip area bone density in postmenopausal women, while conventional training was only able to slow the rate of deterioration. Another more recent study12 found that postmenopausal women who used a vibration platform for five minutes, three times a week for six months, increased their lumbar spine bone density by 2 percent. The control group lost about 0.5 percent of theirs in that same timeframe.
Blood Restriction Training Also Minimizes Injury Risk
Another technique you can try — which is also excellent for the elderly, or athletes recovering from an injury — is blood flow restriction or Kaatsu training. I’ll publish a full-length article on this in the near future but, in brief, it involves performing strength training exercises while restricting venous blood flow (but not arterial flow) to the extremity being worked.
A significant benefit of the method is that you can do strength exercises using just 30 to 50 percent of the weight you’d normally use while still reaping maximum benefits. It’s said blood flow restriction training can stimulate muscle growth and strength in about half the time, using about one-third of the weight, compared to standard weight training.
In the video above, Dr. Jim Stray-Gundersen, a leading proponent and teacher of Kaatsu in the U.S., discusses the method and its benefits. The American College of Sports Medicine claims you need to lift a weight that is at least 70 percent of your single rep max (1RM) to produce muscle growth,13 but studies assessing low-intensity exercise in combination with blood flow restriction have shown you can go as low as 20 percent of 1RM and still reap the benefits.
For most, 20 percent of 1RM is lighter than a warmup, virtually guaranteeing you will not sustain any kind of injury. Indeed, blood flow restriction training is used to rehabilitate the old and infirm in Japan, allowing them to rebuild muscle and regain some of their lost mobility.
Nitric Oxide Dump — A Great Exercise for Aging Muscles
Another exceptionally safe way to improve your muscle strength and general fitness is the nitric oxide dump — a revision and, I think, significant improvement of my Peak Fitness program. Instead of doing 20 minutes’ worth of high-intensity interval training (HIIT) on an exercise bike or elliptical machine, you can reap the same or better benefits doing four simple body movements that take just three minutes.
These exercises should ideally be done three times a day, and do not require weights of any kind. For a full demonstration, see the video above. Even though this exercise is only a few minutes, it will make you short of breath. Please be sure to breathe only through your nose, not your mouth. This is my new favorite high-intensity exercise and, unlike other high-intensity exercises, can be done every day unless you need to recover. Start with 10 repetitions of each movement and work your way up to 20 with the following:
- 10 deep squats, raising your arms parallel to the floor as you squat deeply, getting your butt back as far and as low as possible while still making sure your knees stay behind your toes
- 10 alternating perpendicular arm raises, stopping when your arms are the height of your shoulders
- 10 stationary jumping jack motions. You’re not jumping; just moving your hands overhead, and touching hands on the upper and lower portions of the movement. Make sure your arms come up behind your head and not in front. This requires you to pinch your shoulder blades together
- 10 overhead shoulder presses, making sure to keep your chest out and shoulder blades pinched together
How the Nitric Oxide Dump Can Benefit Your Health
Do each set in rapid succession, without resting in between. When you’re done, you’ll have completed a total of 120 to 240 movements. Done three times a day, with at least two hours in between each session, you’ll end up doing 360 to 920 movements a day. This exercise will:
- Trigger the release of NO, a gas with antioxidant properties that protects your heart by relaxing your blood vessels and lowering your blood pressure, stimulates your brain, kills bacteria and even defends against tumor cells
- Stimulate anabolic muscle building in addition to thinning your blood, making it less likely to clot and improving your immune function. NO is a potent bronchodilator and vasodilator, so it helps significantly increases your lungs’ oxygen-absorbing capacity
- Give you more exercise benefits in a shorter time. You get more benefits from this exercise than you would get from most things you do in a gym in an hour. And, if you do it three times a day, that means you may be getting three to 10 times the metabolic benefit you’d get by going to the gym. Not that going to the gym is unwise; it’s just that your body needs exercise throughout the day
- Stimulate mitochondrial function and health. Mitochondrial decline is closely linked to reduced cardiorespiratory fitness, and decreased resting mitochondrial ATP production may be involved in the development of insulin resistance with aging. By forcing your mitochondria to work harder, exercises such as this one will trigger your body to produce more mitochondria to keep up with the increased energy demand, and promote mitochondrial function and health
Older Adults Benefit From High-Intensity Exercise
While you must certainly start any exercise program at a level appropriate for your current condition, it would be a mistake to dismiss HIIT altogether. Recent animal research suggests HIIT can be safe and effective even in older populations, and may actually help reverse frailty. (As mentioned, the nitric oxide dump exercise is an excellent alternative to other HIIT programs.) As noted by study co-author Dr. Bruce Troen:14
“We know that being frail or being at risk for becoming frail puts people at increased risk of dying and comorbidity. These results show that it’s possible that high-intensity interval training can help enhance quality of life and capacity to be healthy … Increased mitochondrial biomass allows you to utilize oxygen more efficiency [sic]. With HIIT, we saw both mitochondrial increase and an improvement in muscle quality and fiber size in these mice …
Those four mice who had exhibited the kinds of deficits that correlate to frailty in humans improved to a completely robust level. The HIIT actually reversed frailty in them. Because the performance measures for the mice are directly relevant to clinical parameters, we think this program of exercise is quite applicable to humans. We’re laying a foundation so we can do this in people and so we can understand how to tailor it to individuals so they can successfully implement this.
Exercise stresses the system and the body can respond beneficially. We believe that the intensity of individualized HIIT provides a more significant but manageable stress so the body responds more robustly to these short, vigorous periods of exercise. In other words, you get more bang for your buck.”
Other Important Lifestyle Factors That Help Protect Your Bone Health
Getting older doesn’t automatically mean you’ll get weak and frail. Your lifestyle plays a decisive role here, and exercises such as those discussed above are effective means by which you can prevent osteoporosis. That said, you’ll also want to pay attention to your diet.
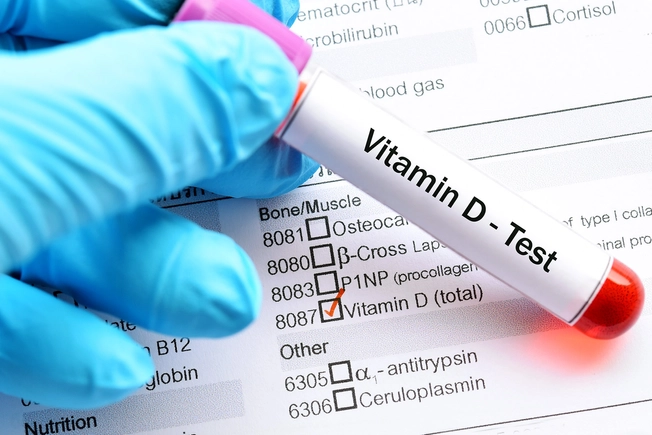
Processed foods produce biochemical and metabolic conditions in your body that decrease bone density over time, so avoiding processed foods is definitely an important part of the equation. Certain nutrient deficiencies can also contribute to weak and brittle bones. Among the most important are animal-based omega-3 fats, calcium, vitamins D and K2, along with magnesium. Following is a summary of some of the most important general guidelines for maintaining or increasing your bone strength:
• Avoid processed foods and soda, which can increase bone damage by depleting your bones of calcium. By ditching processed foods, you’re also automatically eliminating a major source of refined sugars and processed fructose, which drive insulin resistance. It will also provide you with a more appropriate potassium-to-sodium ratio, which is important for maintaining bone mass.
• Increase your consumption of raw, fresh vegetables, ideally organic. If you find it difficult to eat the recommended amount of vegetables you need daily, you can try vegetable juicing.
• Optimize your vitamin D levels, ideally from appropriate sun exposure. Vitamin D builds your bone density by helping your body absorb calcium. If you use an oral supplement, make sure you’re using vitamin D3 (not D2), and that you’re also increasing your vitamin K2 intake.
Consider making your own fermented vegetables using a special vitamin K2-producing starter culture, or supplementing with vitamin K2 if you’re not getting enough from food alone. Vitamin K2 serves as the biological “glue” that helps plug the calcium into your bone matrix. Also remember to balance your calcium and magnesium (1-to-1 ratio).
• Avoid sitting and incorporate as much nonexercise movement into each day as possible.
• Get regular exercise. Ideally, your fitness program should be comprehensive, providing the necessary weight-bearing activities for bone health while also improving your cardiovascular fitness and fat-burning capabilities with high-intensity exercises, along with gentle balance- and flexibility-boosting exercises such as yoga, Qigong and Tai Chi.
.jpeg)