While AID has traditionally been used in type 1 diabetes, new data suggests this technology has many of the same benefits in type 2 – namely, improving time in range and A1C while reducing hypoglycemia. Plus, AID dramatically simplifies blood sugar management.
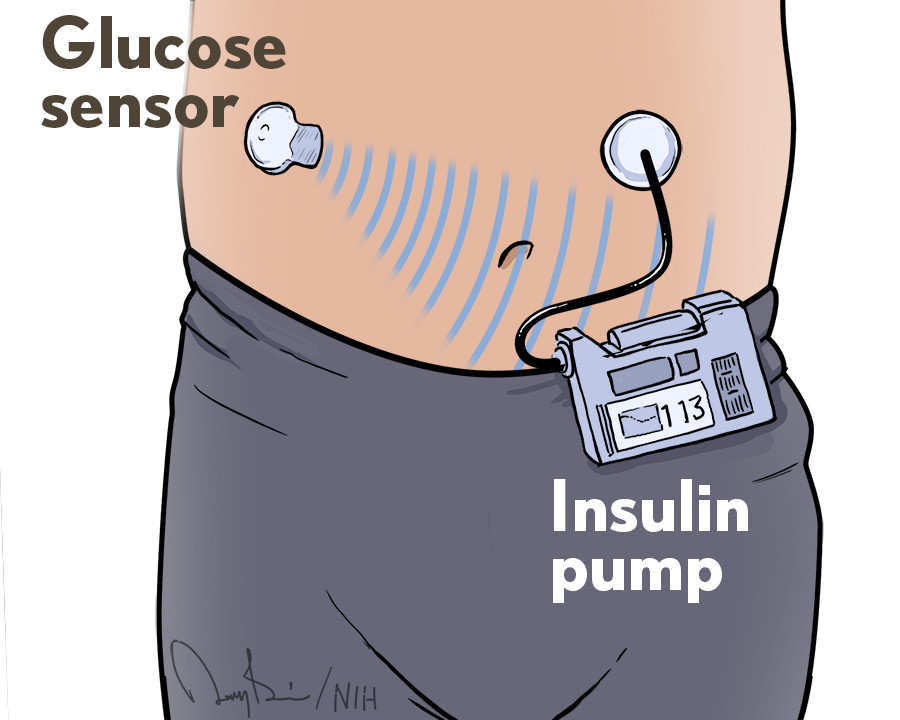
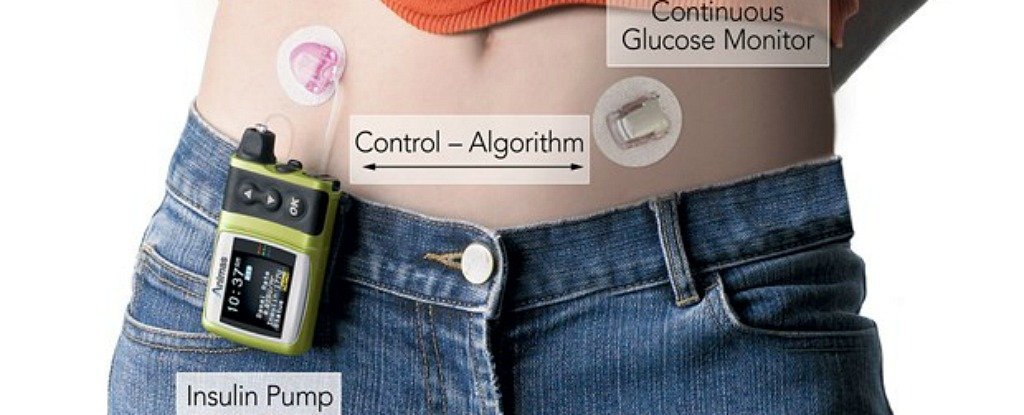
From continuous glucose monitoring (CGM) to automated insulin delivery (AID) systems, diabetes technologies that began as innovations for people with type 1 diabetes are slowly beginning to reach people with type 2.
For instance, many insurance companies now cover CGMs for people with type 2 diabetes who take insulin as well as those who are not on insulin but have a history of hypoglycemia. And earlier this week, the FDA approved Stelo by Dexcom, a CGM designed specifically for people with type 2 diabetes who are not taking insulin.
However, less progress has been made with reimbursement by insurance companies for AID. Off-label use of AID drew significant attention at the ATTD 2024 conference, with presenters highlighting the benefits for many people with diabetes across a range of settings and systems.
AID improves time in range across different systems and settings
Research shows that AID leads to many of the same benefits in type 2 diabetes as in type 1 diabetes: improved time in range, reduced hypoglycemia, and reduced A1C. Importantly, these benefits were consistent across different study settings and regardless of which AID system was used.
A study of 30 Tandem Control-IQ users with type 2 diabetes found that time in range increased by about 15% from 56% at baseline to 71% at six weeks. This translates to an increase of 3.6 hours per day spent in range.
Dr. Anders Carlson, diabetes medical director at the International Diabetes Center in Minnesota, said this finding is in line with studies in type 1 diabetes as well as the time in target range guidelines for type 1 diabetes.
Outside of clinical trials, research suggests that the benefits of AID extend to people with type 2 diabetes in the “real world.”
In a study presented at ATTD, MiniMed 780G users were able to achieve 71-75% time in range outside of a clinical trial, again meeting the targets for diabetes. “This is really compelling evidence that in a real-world setting, this AID system can work for people with type 2 diabetes,” Forlenza said.
Participants who used the recommended MiniMed 780G settings (i.e. the lowest glucose target) achieved a time in range of 80%.
For Carlson, this finding raises an important question – what are the optimal settings for AID in type 2 diabetes? For instance, since low blood sugar (hypoglycemia) is less of a concern, it may be beneficial to have more aggressive targets from the get-go.
Another study investigated the Omnipod 5 AID system in 24 participants with type 2 diabetes, finding strong improvements in time in range with minimal hypoglycemia. Among those on MDI, time in range increased from 43% at baseline to 58% at six months. Participants on basal insulin only saw even larger improvements in time in range, from 31% at baseline to 65% at six months.
Dr. Anne Peters, professor of medicine at USC, also highlighted reductions in total daily insulin dose among participants on MDI – yet another way in which AID could simplify type 2 diabetes management.
How might combining AID with GLP-1s and SGLT-2s affect glucose levels?
Growing use of GLP-1 receptor agonists, SGLT-2 inhibitors, and diabetes technology poses new questions for the future of diabetes care. That is, how might the combination of technology and medications optimize outcomes for people with type 2 diabetes?
In the Omnipod 5 study, half of the patients were also taking a GLP-1 or SGLT-2. Overall, Omnipod users taking a GLP-1 or SGLT-2 saw greater improvements in time in range compared to those who were only taking insulin. Participants in the GLP-1 or SGLT-2 group saw a 24% increase in time in range from 28% at the start of the study to 62% at eight weeks. Meanwhile, participants not using a GLP-1 or SGLT-2 improved their time in range by 18%, from 35% at baseline to 53% at eight weeks.
Carlson said this finding suggests that combining GLP-1s or SGLT-2s with AID could potentially lead to even better glycemic control than AID alone – though formal studies will be needed to test this hypothesis.
Similarly, Dr. Gregory Forlenza, associate professor of pediatric endocrinology at the University of Colorado, noted the ability of GLP-1s to reduce insulin needs. Combining these powerful medications with AID may help people with type 2 diabetes improve glycemic control and lose weight. It’s possible these improvements could even help people work toward diabetes remission.
What about AID for older adults with type 2 diabetes?
Starting insulin can be challenging for people of all ages, but it can be especially complex for older adults or disabled people with type 2 diabetes who receive home care.
Elderly people have a higher risk of severe hypoglycemia and hypoglycemia or ketoacidosis. Diabetes management for older adults can also be complicated by impaired cognition or dementia, reduced mobility, and difficulty accessing care.
In this context, the CLOSE AP+ study investigated AID assisted by nurses in people with type 2 diabetes unable to manage their own multiple daily injections (MDI) at home. CLOSE AP+ tested Control-IQ technology in 25 participants who had an average age of 70 years.
At 12 weeks, time in range improved significantly, from 37% to 63%. Time below range was less than 1%, while time above range was under 10%. Overall, Reznik highlighted that a majority of participants reached the American Diabetes Association guidelines for older people with diabetes. These guidelines recommend:
- At least 50% time in range (70-180 mg/dL)
- Less than 1% time below range (<70 mg/dL)
- Less than 10% time above range (>250 mg/dL)
It’s also worth noting that participants using Control-IQ technology saw a significant 1.3% reduction in A1C. Over 90% of participants reached an A1C of less than 8% by the end of the trial, without any increase in severe hypoglycemia. Dr. Yves Renzik, professor of endocrinology at CHU Caen Normandy in France, also highlighted high patient confidence and high nurse satisfaction with the AID system in this study.
Ultimately, the CLOSE AP+ study showed that AID can be used safely in people with type 2 diabetes who require home nursing care. This confirms the benefits of AID extend beyond the “standard” person with type 2 diabetes to older adults and people with disabilities.
The bottom line
Numerous presentations at ATTD 2024 demonstrated that AID is safe and effective for people with type 2 diabetes. Both clinical trials and real-world data show that this technology increases time in range and improves A1C while minimizing hypoglycemia.
“I want to emphasize that across a wide variety of real world and clinical trial evidence sets, and across very different AID systems, everyone is either doing a great job hitting a goal for time in range or achieving a massive improvement in glucose control,” Forlenza said. He noted that AID leads to time in range increases of 15% to 24% in people with type 2 diabetes, nearly double the improvements typically seen in type 1 diabetes.
However, several questions remain to be answered regarding optimal settings, bolusing, and the potential of AID when combined with GLP-1s and SGLT-2s. Carlson highlighted the following areas for further research:
- Are people on MDI the only candidates for AID? Or could AID be used in all people with type 2, regardless of their insulin needs and whether or not they’re meeting glycemic goals?
- Is previous experience with technology necessary for successful use of AID in people with type 2 diabetes?
- Does AID help with diabetes self-management (such as carb awareness)?
- What role will primary care providers provide in supporting AID in this population?
Beyond glycemic data, it’s also important to consider user experience with AID. Overall, the data suggests that people with type 2 diabetes had good satisfaction and confidence in using these systems. Even people who hadn’t previously used diabetes devices reported a positive experience with AID, Peters noted.
“I honestly wasn’t sure my patients would like AID – many were technology-naive people,” Peters said. “But they loved it and they wanted to stay on it because they felt it improved their glycemic control.”