To stem the rising tide of antimicrobial resistance, innovative companies are racing to develop new therapeutics, vaccines, and monitoring tools
When we turn our attention to emerging global threats, we know what to expect: grim statistics, dire predictions, and—perhaps worst of all—disturbing revelations that no preventive or corrective actions commensurate with the threats have been mustered. The threat we know as antimicrobial resistance (AMR) is no exception.
Consider this warning from the United Nations: “According to recent estimates, in 2019, 1.27 million deaths were directly attributed to drug-resistant infections globally. By 2050, up to 10 million deaths could occur annually. If unchecked, AMR could shave $3.4 trillion off GDP annually and push 24 million more people into extreme poverty in the next decade.”
Grim statistics? Check. Dire predictions? Check. And what about revelations that preventive or corrective actions have been insufficient? Well—as much as we might hate to admit it—Check.
According to the World Health Organization (WHO), its own Global Action Plan on Antimicrobial Resistance, a plan endorsed by the World Health Assembly in 2015, isn’t being realized: “Although antimicrobial resistance is recognized as a global threat requiring urgent action, over the past six years little progress has been made in improving awareness of antimicrobial resistance, monitoring antimicrobial consumption, implementing infection prevention and control programs, and optimizing antimicrobial use in the human sector.”
The WHO has also complained that there has been little progress on yet another action item—the development of new medicines, vaccines, and other interventions. Here, the WHO suggests that the problem is “market failure.” This is a well-known problem, particularly with respect to the development of new antibiotics. New antibiotics are so few and so important as a last resort that they must be administered sparingly lest they, like so many older antibiotics, become useless through overuse and concomitant induction of antibiotic resistance.
The economic disincentives are clear. Why commit to developing antimicrobials if they are to be used sparingly, which has the effect of limiting sales volumes? Also, antimicrobials are typically administered infrequently (in the case of vaccines) or for short durations (in the case of therapeutics), further limiting sales volumes. Yet some companies, a few of which appear in this article, are undeterred. They are optimistic about developing new antibiotics, vaccines, and phage therapies to combat antimicrobial resistance.
Working to bring new antibiotics to the market
Lyndsay Meyer, director of U.S. Corporate Communications at GSK, emphasizes that the company has been developing antibiotics for over 70 years: “We are building off our long and successful history in this space by developing innovative vaccines and medicines for bacterial and fungal infections.” She notes that GSK currently has more than 30 R&D projects relevant to antimicrobial resistance.
Meyer stresses that GSK is one of the few companies that is actively developing new classes of antibiotics. “Newer antibiotics are used sparingly to curb antibiotic resistance—and rightly so,” she explains. “However, this makes it a struggle for companies to turn a profit.”
She emphasizes that gepotidacin—which already met its primary efficacy endpoint in GSK’s recent Phase III trials—could become the first novel oral antibiotic treatment for uncomplicated urinary tract infections in over 20 years. This novel drug inhibits bacterial DNA replication by a distinct mechanism that involves independent binding to two different type II topoisomerase enzymes.
Gepotidacin provides activity against most strains of Escherichia coli, including isolates that are highly resistant to current antibiotics. What makes the drug so effective is the way it independently binds to two different enzymes, which would require the bacteria to develop mutations in both enzymes to become resistant to the drug.
Meyer notes that GSK also has an exclusive license agreement with Spero Therapeutics for another antibiotic to treat complicated urinary tract infections—tebipenem pivoxil hydrobromide (tebipenem HBr). She explains that the drug belongs to a class of antibiotic agents called carbapenems, which are typically reserved for severe bacterial infections or suspected multidrug-resistant bacterial infections.
Developing vaccines for difficult-to-treat conditions
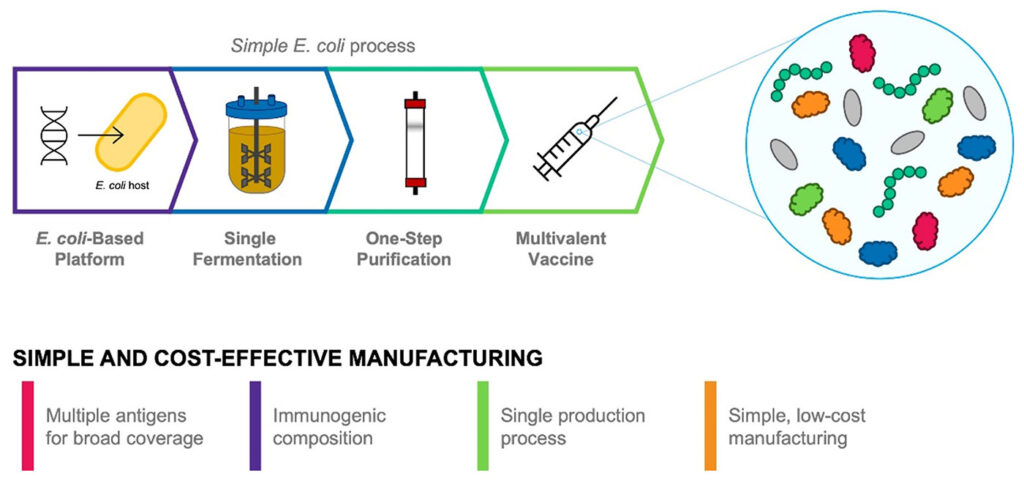
At LimmaTech Biologics, CSO Michael Kowarik, PhD, and COO Patricia Martin, PhD, believe that vaccines help minimize antimicrobial resistance by preventing drug-resistant infections in the first place. They also believe that vaccines are advantageous because they are specific to individual pathogens. As a result, they do not harm the natural microbiome that is so critical to human health.
Kowarik highlights that LimmaTech is developing a pipeline of vaccine candidates that target gonorrhea, shigellosis, and other yet-to-be-disclosed indications.
He explains how Neisseria gonorrhea, the bacterium responsible for gonorrhea, is now showing resistance to multiple classes of antibiotics: “The problem with this pathogen is that it has developed multiple decoy mechanisms to evade the immune system. For example, it exhibits significant variation in the antigens on its surface proteins and can easily alter its surface structure during infection.”
LimmaTech is developing a vaccine candidate against N. gonorrhea that is currently in preclinical testing. “To target this issue of surface variability,” Kowarik notes, “our gonorrhea vaccine candidates contain multiple immunogenic antigens that are invariable—or conserved—and not altered during infection.” He adds that these antigens can be produced in a single-step process, which streamlines the development timelines of the vaccine and improves cost-effectiveness.
Martin reports that the company is also working on vaccines against Shigella bacteria, which are responsible for shigellosis. “Shigellosis is a major cause of inflammatory diarrhea that results in over 200,000 deaths every year,” she points out. “Compounding the problem, multidrug resistance in Shigella bacteria is rising dramatically.”
She says that LimmaTech is currently evaluating the safety and immunogenicity of a Shigella vaccine candidate in a Phase I/II clinical trial in Kenyan children. She notes that the vaccine was developed using a technique called bioconjugation. This technique is necessary because the polysaccharides on the surface of Shigella species do not always elicit a strong immune response.
“At the core of our approach,” she details, “is a bacterial enzyme that forms precise linkages between surface polysaccharides and an immunogenic protein.” The Shigella vaccine is tetravalent, that is, it incorporates four antigens. It covers up to 85% of diseases produced by Shigella.
Using bacteriophages to target specific bacteria
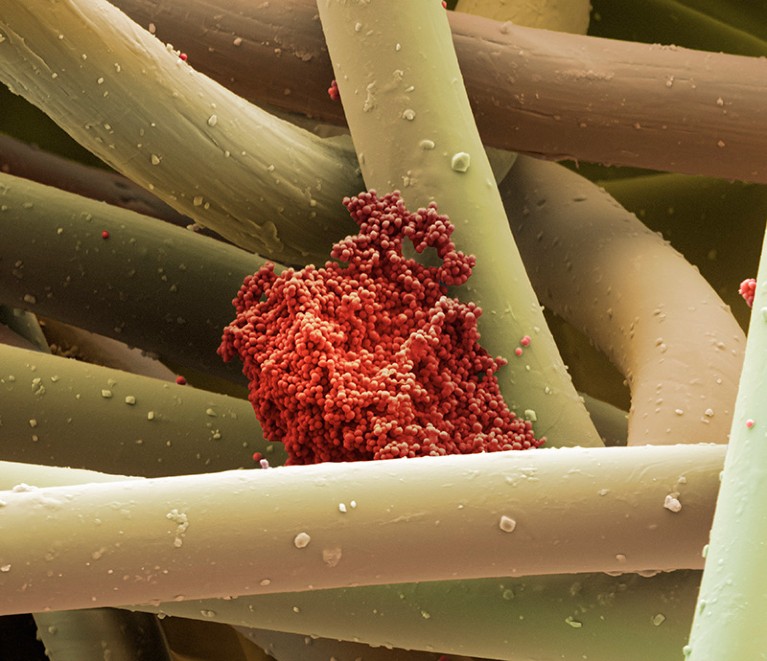
Cocktails or fixed combinations of engineered bacteriophages are being developed by Locus Biosciences to combat the development and spread of antibiotic resistance. Locus’s cocktails are designed to target specific conditions such as urinary tract infections. According to the company, these cocktails can target over 95% of the bacteria causing an infection.
A bacteriophage—which means bacteria eater in Greek—is a virus that preys on bacteria. “The major advantage of bacteriophages over traditional antibiotics is their ability to target and kill the specific bacteria causing the infection,” says Paul Garofolo, the co-founder and CEO of Locus Biosciences. “This leaves the good bacteria—the so-called healthy microbiome—unaffected.
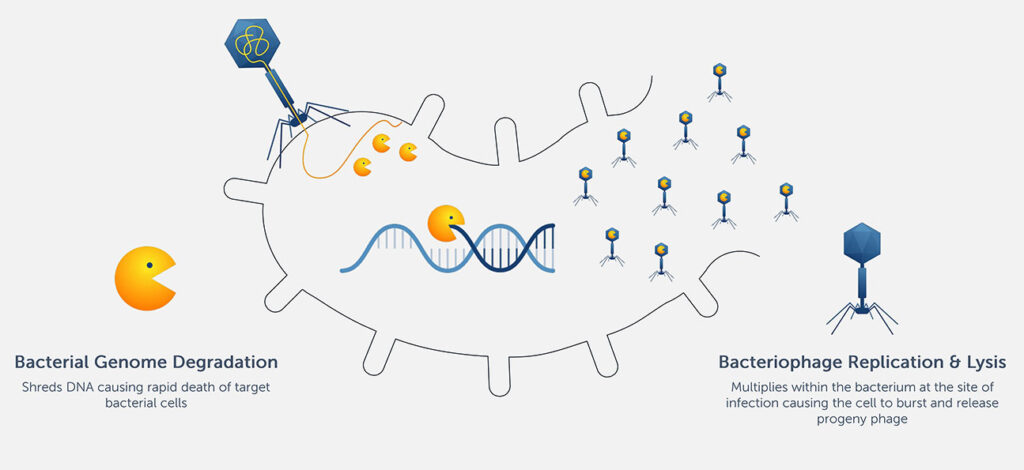
cell lysis.
Locus suggests that its bacteriophage cocktails would be suitable as an early-use option in the treatment of antibiotic-resistant infections—as opposed to a last-line option. Garafolo asserts, “Following the diagnosis of a specific condition like a urinary tract infection, our fixed phage cocktails allow a doctor to pull the drug right off the shelf and use it when it’s needed.”
Garofolo says that Locus’s phages are modified to encode a bacterial genome–targeting CRISPR construct. When the phages infect bacteria, the array is transduced into the bacterial genome, where elements of the construct are expressed that kill the bacterium. One of these elements is Cas3. Unlike the more familiar Cas9, which works like a pair of scissors, Cas3 acts more like a shredder.
“Cas3 and Cas9 differ in what they do upon recognizing a DNA sequence in the bacterial genome,” Garofolo elaborates. “While Cas9 makes a clean cut in DNA, Cas3 degrades thousands to tens of thousands of base pairs. Cas3 ensures the death of the bacterial cell.”
Thus far, Locus’s approach has an impressive safety record, with the FDA designating multiple phage products as GRAS or generally regarded as safe for several food safety applications. For pharmaceutical products, Garafolo says that Locus is beginning to conduct clinical trials.
Locus is currently in the middle of a Phase II trial for its lead bacteriophage therapy, LBP-EC01, an engineered fixed cocktail of CRISPR-Cas3-enhanced bacteriophages targeting drug-resistant urinary tract infections caused by E. coli. The company also has preclinical programs targeting Klebsiella pneumoniae, Pseudomonas aeruginosa, and Staphylococcus aureus. “Together,” Garafolo declares, “these are four of the top bacterial species contributing to the multidrug resistance threat worldwide.”
Software for alerting hospitals of infectious outbreaks
Sam Sihvonen, the co-founder and CEO of Solu Healthcare, notes that Solu means cell in Finnish. The Helsinki-based company is developing a real-time microbial database to monitor how bacteria, viruses, and fungi evolve over time. “Our easily accessible data,” Sihvonen asserts, “can be used to improve the diagnosis and treatment of hospital infections, saving money and lives.”
Solu has developed novel software-based algorithms that alert hospitals about which antibiotic-resistance genes are found in outbreaks. According to Sihvonen, Solu’s algorithms make use of existing resistance databases that the scientific community has developed over the past few decades.
Solu’s genomic analysis algorithms are based on raw data from whole genome sequencing. Whole genome sequencing—which uses various commercial technologies to extract DNA and produce the final sequence—is very effective at identifying causative variants for follow-up studies.
“The great thing about whole genome sequencing is that you can capture all existing variants, including new genetic variants,” Sihvonen explains. “This is not possible with a lot of targeted PCR approaches and phenotypic screening methods.” Furthermore, he stresses that the technique can now be performed within hours, a key requirement for Solu’s technology.
Sihvonen says that a lot of information can be obtained from Solu’s algorithms. For instance, they can identify the species and strains of bacteria. They can also determine which antimicrobial resistance genes are found in a sample.
Finally, Solu’s algorithms can elucidate how different outbreaks are linked. “For instance,” Sihvonen points out, “they can provide information about whether Patient A infected Patient B or Patient C. Information like this needs to be quickly uncovered once outbreaks are suspected in hospitals.”
Future of antimicrobial resistance
Sihvonen stresses that rapid bacterial evolution and natural selection in microorganisms will probably always be a problem. He concludes that “it is unlikely that we are ever going to completely eradicate antibiotic resistance.” Furthermore, Garofolo predicts that antibiotics will continue to form the bedrock of modern medicine in the foreseeable future. He adds, however, that he thinks “the goal will be to complement traditional antibiotics with novel medicines like phage treatments and vaccines.”




 Antimicrobial resistance is a growing problem worldwide
Antimicrobial resistance is a growing problem worldwide
Comment
Historically, antimicrobial resistance in Neisseria gonorrhoeae emerged in Asia and then spread to other countries including the U.S., usually first in Hawaii or the West Coast (N Engl J Med 2012; 366:485). Because gonorrhea is now mostly diagnosed through nonculture methods such as NAATs, surveillance for antimicrobial susceptibility is a public health priority. The CDC’s GISP surveillance system, set up in 1986, has found fewer than 1.5% of isolates with reduced susceptibility to ceftriaxone (defined as MIC ≥0.125 µg/mL) and none with resistance, defined as an MIC ≥0.25 µg/mL (MMWR Morb Mortal Wkly Rep 2016; 65:1). Now that a ceftriaxone-resistant N. gonorrhoeae isolate has been identified in North America, clinicians must be vigilant and consider performing a culture in cases where the infection was acquired in Asia or, like in this case, when the patient had sexual contact with someone who had unprotected intercourse in Asia.