Drug combination enhanced delivery of antibacterial medications in rabbits
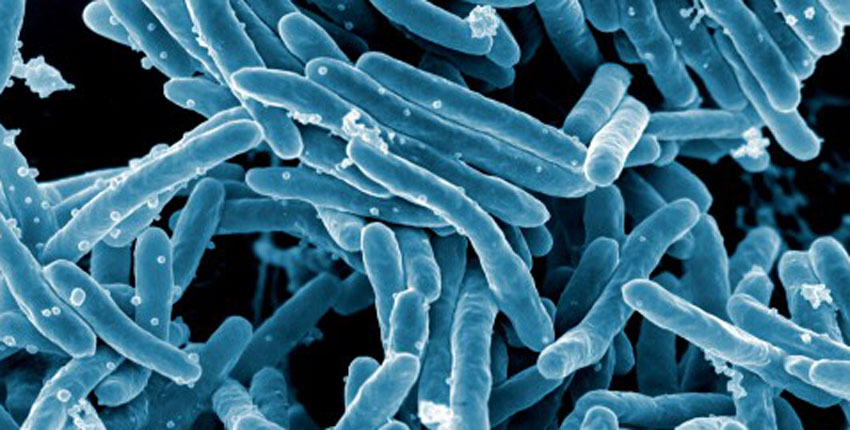
Mycobacterium tuberculosis bacteria.
At a glance:
- A combination of approved cancer drugs may improve tuberculosis treatment.
- In a rabbit model of tuberculosis, the repurposed drugs enhanced delivery of antibacterial medications.
- The drugs also promoted antibacterial responses and improved health outcomes in the animals.
- Next, the combination would need to be tested in patients with tuberculosis.
Researchers have identified a combination of existing cancer drugs that may improve treatment for tuberculosis.
In a study conducted in rabbits and led by Harvard Medical School researchers at Massachusetts General Hospital, the repurposed drugs enhanced delivery of antibacterial medications that target tuberculosis-causing bacteria. Findings published March 27 in PNAS.
Although it is often overlooked in industrialized countries such as the United States, tuberculosis remains one of the deadliest diseases globally, causing millions of deaths every year.
Sometimes, patients die even after being treated, either because tuberculosis bacteria develop resistance to antibacterial drugs or because the ability to deliver medications to infected lung tissue is poor.
To address the latter challenge, researchers repurposed a pair of cancer drugs already approved by the U.S. Food and Drug Administration. The drugs were originally designed to enhance drug delivery to cancer cells by improving the structure and function of blood vessels around tumors, which can be compromised in cancer.
Blood vessel integrity is also an issue in tuberculosis: Often, the disease results in poorly functioning vessels and an overabundant extracellular matrix — the network of proteins and other molecules that surround and give structure to tissues. As a result, blood flow and drug delivery can be reduced in the abnormal lung masses where tuberculosis bacteria reside, allowing the bacteria to evade the body’s immune system.
“Our team is interested in understanding and overcoming physiological barriers to drug delivery” in tuberculosis lung masses, said senior author Rakesh Jain, the Andrew Werk Cook Professor of Radiation Oncology at HMS. “Even the most potent antibacterial drug will fail if it cannot reach the bacteria fueling the disease.”
A multidisciplinary team of engineers, cancer biologists, immunologists, microbiologists, and data analysts used a rabbit model of tuberculosis to test two drugs known as host-directed therapies, or HDTs. One, bevacizumab, acts on blood vessels, and the other, losartan, targets the extracellular matrix.
Previously, Jain and colleagues showed that bevacizumab could improve antibacterial drug delivery to tuberculosis lung masses. Now, they’ve shown that combining bevacizumab with losartan enhances this drug delivery, promotes antibacterial responses, and improves health outcomes. Surprisingly, the HTDs reduced bacteria numbers in lung masses even without antibacterial agents.
To identify the mechanisms involved, the investigators analyzed tuberculosis lung masses and other lung tissue. They found that the HDTs promoted inflammatory responses to tuberculosis bacteria in immune and nonimmune cells.
Also important, bevacizumab and losartan are approved, safe, and affordable, Jain said, so the study lays the groundwork for directly translating the results into the clinic.
A next step, he added, would be “to test these HDTs in patients with tuberculosis for the drugs’ ability to improve outcomes of antibacterial therapy.”