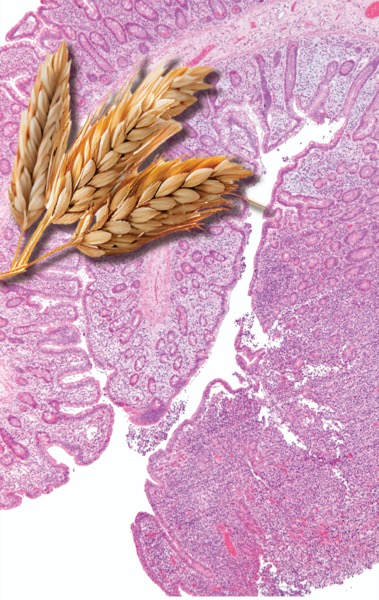
VANCOUVER, B.C.—The incidence of enteropathy-associated T-cell lymphoma—a rare and aggressive T-cell, non-Hodgkin lymphoma—is rising, according to data presented at the 2023 annual meeting of the American College of Gastroenterology.
The growing number of EATL cases could be connected to the increase in celiac disease, given the strong association between the two conditions, researchers said.
“Although [EATL is] rare, most of the cases that we see develop in patients with celiac disease,” said lead investigator Isabel Hujoel, MD, the clinic director of the Celiac Disease Center at UW Medical Center, in Seattle. “We don’t know why the incidence of EATL has steadily risen over the past two decades, but we suspect that it’s because celiac disease continues to increase in prevalence.”
The study, which used the Surveillance, Epidemiology, and End Results (SEER) program database, found 463 cases of EATL between 2000 and 2020, with an age-adjusted incidence rate of 0.014 per 100,000 people (abstract P1249). However, the incidence of EATL increased by 2.58% annually over this 20-year period.
Poor Survival Outcomes
Findings from the study, which won Presidential Poster and Outstanding Research Awards, also showed that EATL was more common in men, and that the median age at diagnosis was 65 years. Most cases (42%) were treated with both surgery and chemotherapy.
Older age at the time of diagnosis was associated with a higher risk for death, while factors such as sex, race, year of diagnosis and time to treatment initiation showed no significant impact on survival.
Notably, despite medical advances over the past two decades, the data showed no change in survival over the study period. “Unfortunately, survival outcomes of patients with EATL have not improved over time,” Dr. Hujoel said. “Mean survival for this disease remains approximately six months.”
A separate, retrospective cohort analysis of 259 patients in the SEER database found that the majority of patients underwent surgical resection (69.9%), followed by chemotherapy (47.5%) (abstract P1594).
Investigator Sophia Dar, MD, a gastroenterology fellow at Southern Illinois University School of Medicine, in Springfield, told Gastroenterology & Endoscopy News that treatment with these methods was associated with improved survival rates compared with no treatment. Chemotherapy alone also decreased the hazard ratio when compared with no treatment.
“Patients in the chemotherapy group marginally outperformed their surgical counterparts, indicating perhaps chemotherapy as a more viable treatment option in certain scenarios,” Dr. Dar said. “Unfortunately, irrespective of treatment, 83.7% of patients died in the five-year follow-up period.”
Researchers from both studies emphasized the need for further study, especially considering the strong association between EATL and celiac disease.
“Better understanding of the factors contributing to the high mortality rate could help medical practitioners develop more efficient treatment plans for EATL,” Dr. Dar concluded.
Screen Only for Refractory Disease
Debra Silberg, MD, PhD, the chief scientific officer of the nonprofit Beyond Celiac, based in Ambler, Pa., told Gastroenterology & Endoscopy News that the research does not address whether the increase in EATL is accounted for by patients with celiac disease, but “since there has also been an annual increase in celiac disease diagnosis, it follows that there would be an increase in EATL. Therefore, the overall percentage of EATL in patients with celiac disease may not have changed—which is around 0.22 to 1.9 per 100,000—and is still extremely rare,” she added.
Regarding screening, Dr. Silberg referred to the American Gastroenterological Association guidelines for refractory celiac disease (Gastroenterology 2022;163[5]:1461-1469). If a patient is diagnosed with type 2 refractory celiac disease, which, she said, “is associated with clonal T-cell expansion, then small bowel imaging is recommended to exclude EATL and ulcerative jejunoileitis. Since EATL is still rare even with this increased incidence,” she added, “only patients with refractory celiac disease or a suspicion of a complication of celiac disease should be screened.”