
For decades, the answer to lowering cholesterol to prevent heart attack or stroke was a statin prescription. Unfortunately, many people prescribed statins stop taking them due to side effects, while others question their efficacy. One study even found that doctors have overprescribed statins worldwide, which can potentially be harmful.
Is statin therapy suitable for you? A simple test could give you a better idea of your risk for a heart attack or stroke by evaluating your coronary artery calcium (CAC) score.
‘Bad’ Cholesterol May Not Be Bad
Both the media and food industry tout the importance of a low-cholesterol diet, and we often hear about “bad” and “good” cholesterol.
The “bad” cholesterol is the low-density lipoprotein cholesterol (LDL-C), and the “good” cholesterol is the high-density lipoprotein cholesterol (HDL-C).
It’s important to note that without cholesterol, we could not survive.
It helps make up our cells and hormones, it’s crucial in the delivery of insulin into our cells, and it helps make up the essential vitamins A, D, E, and K.
The “bad” cholesterol is not necessarily bad. It is theorized that one of LDL-C’s primary jobs in the bloodstream is to help repair artery walls from the damage caused by inflammation and bacteria. But once the LDL-C builds up along artery walls over time, it can form hard calcium plaques that block blood flow to the heart, ultimately causing a heart attack.
That’s why yearly blood tests usually include a fasting cholesterol level with a breakdown of LDL, HDL, and triglycerides.
The goal is for LDL to be below 100, HDL to be above 60, and triglycerides below 100. Doctors often prescribe a statin when these numbers stray from the norm.
Statin Therapy
In 1987, the U.S. Food and Drug Administration (FDA) approved the first cholesterol-lowering medication, lovastatin.
Since then, several other statin medications have been developed by various drug companies, all claiming to lower the risk of heart attack and stroke by reducing cholesterol levels in the blood.
In 2018, an estimated 145.8 million people worldwide took statins, and between 2002 and 2018, an average of 21.35 million statins were purchased annually with an average cost of $24.5 billion.
Throughout the years, the efficacy and safety of statin medications have come into question. Many people prescribed statins stopped taking them due to side effects, including:
- Muscle weakness
- Rhabdomyolysis ranging from mild to life-threatening
- Liver dysfunction
- Onset of diabetes mellitus
- Acute kidney injury
- Memory loss and poor cognition
Nearly all statin drugs are associated with musculoskeletal side effects. Myalgia is the most common symptom, and myositis is less common and associated with a rise in creatine kinase (CK). Rhabdomyolysis is the most severe musculoskeletal form observed, with a rise in CK greater than 10 times the upper limit of normal, with associated features including myoglobinuria, renal impairment, and serum electrolyte abnormalities.
Others question whether statins reduce heart attack and stroke risk more than a healthy diet and regular exercise.
At least one study has even claimed statins can harm many individuals and are over-prescribed.
In 2019, the American Heart Association (AHA) developed new guidelines about the primary prevention of cardiovascular disease, advising doctors to consider all risk factors rather than simply looking at cholesterol levels.
When risks are unclear, or if a patient’s bloodwork shows an elevated LDL-C but otherwise minimal risk factors, AHA guidelines direct physicians to consider the CAC score before deciding on statin therapy.
When You May Not Need Statins
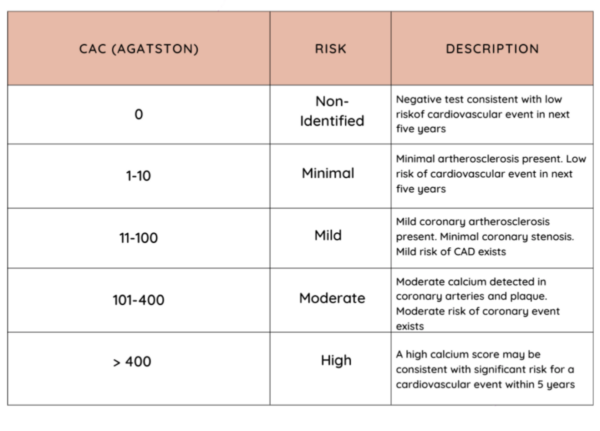
A CAC score measures the extent of calcified plaque in the coronary arteries with a heart CT scan.
It is also known as the Agatston Score, named after Dr. Arthur Agatson, who developed the technique for measurement in the 1990s while working at Mount Sinai Hospital in Miami Beach, Florida.
The hospital had purchased an ultrafast CT scanner that could freeze the motion of the heart to give a clear picture and, ultimately, images of calcium deposits inside the coronary arteries. Agatston created the scoring system by categorizing the risk of heart attack or stroke according to the number and size of calcium plaques in the coronary arteries.
While Agatston worked on his new CAC scoring system, the Framingham Heart Study (FHS) was the gold standard for cardiovascular disease risk measurement. It considered age, gender, LDL-C, family history of heart disease, diabetes, and obesity. Statins were also becoming more readily available, and the medical community hailed them as the answer to reducing the risk of heart attack and stroke by controlling cholesterol.
Agatston, however, wasn’t convinced and was motivated by the realization that everyone with elevated cholesterol didn’t need to take statins. Statins were unnecessary if cholesterol was high, but the CAC score was zero.
Agatston believes up to 50 percent of people who took a statin because of their high cholesterol level didn’t need them after finding their CAC score was zero.
He also notes that several other people with normal cholesterol and no symptoms of cardiovascular disease had a high CAC score revealing severe disease which needed aggressive intervention.
How to Read CAC Score
Agatston suggests men over 40 and women over 50 receive testing, and even earlier if they have a strong family history of cardiovascular disease.
If the scan shows a CAC score of zero, there is no risk of a heart attack, and regardless of whether the LDL-C is high, there is no need for statin therapy.
He suggests a follow-up CT scan after five years.
However, insurance doesn’t cover the CT scan to determine a CAC score, and the average cost of the test is $75 to $150.
Dr. Hillel Wirsztel, an internist at Saint Francis Hospital in Wilmington, Delaware, still prescribes statins for patients with risk factors like diabetes and a family history of cardiovascular disease. Still, he says, “I don’t look at cholesterol. Even before the new guidelines, I wouldn’t prescribe a statin simply because the cholesterol level was high.
“The risk factors are more important, especially as patients get older,” he said.
Wirsztel agrees that having a CT scan to assess a CAC score can be an essential tool and is underutilized, particularly in the United States, where preventative medicine is often not of primary concern.