
)
We all know the feeling of an expanded stomach after a particularly indulgent meal. But beyond the occasional bloating experience, nearly a third of the U.S. population experiences chronic bloating [1]. So what’s behind this symptom when it’s more frequent?
Key Takeaways
- Stress can lead to bloating by increasing inflammation and causing gut bacteria imbalances.
- Irritable bowel syndrome (IBS) symptoms, including bloating and abdominal distention, are strongly associated with stress levels.
- Non-gut-related issues, like pelvic floor dysfunction, can cause chronic bloating.
- Bloating and other gastrointestinal (GI) symptoms can be easily treated with lifestyle and dietary changes, probiotics, and physical therapy.
If you’ve been going through a lot more stress than usual lately, you may have noticed a worsening in your symptoms. And you wouldn’t be wrong, as the research shows that increased stress can worsen bloating and stomach distention.
The link between stress and increased IBS symptoms like bloating is well-established. This is likely due to stress changing the gut microbiota, leading to dysbiosis and/or bacterial overgrowth. These gut flora changes can lead to excess gas production and inflammation inside the GI tract. Unfortunately, as inflammation levels increase, our pain sensitivity also increases, adding to the sensation of bloating.
Fortunately, dietary, lifestyle, and supplemental recommendations are effective at reducing the underlying causes of stomach bloating. This article will take you through some of the most common causes of bloating that result from stress, and will give you a step-by-step guide to alleviating this uncomfortable symptom.
Can Stress Cause Bloating?
Stress can disrupt the normal gut microbiome, creating intestinal dysbiosis and bacterial overgrowth. These changes can lead to digestive symptoms, including bloating. This may be due in part to excess gas production that may cause the sensation of bloating and physical distention, though the exact mechanism hasn’t been confirmed by research.
Additionally, it appears that stress creates an increased perception of bloating, though the exact reason is not well understood [2]. Stress likely causes inflammation in the digestive tract that increases pain receptors, creating more distress related to bloating.
What Is Bloating?
Bloating is the subjective feeling of pressure or gas in the abdomen. It’s important to note that this is different from distention, which refers to the physical expansion of the abdomen [1]. However, these symptoms often present together, and over half of the people who experience bloating also report abdominal distention [1].
Bloating may exist as a symptom on its own, without other signs of GI disturbance. However, it often presents alongside other GI disorders, such as:
- Irritable bowel syndrome (IBS) [1]
- Inflammatory bowel disease (IBD) [3]
- Small intestine bacterial overgrowth (SIBO) [1, 2, 4, 5]
- Chronic constipation [1]
- Dyspepsia and indigestion [1]
- Exocrine pancreatic insufficiency (EPI) [1, 2, 6, 7]
- Gastroparesis [1, 2]
- Gallbladder dysfunction [8]
- Stomach ulcers [9]
- Chronic overeating [5]
Occasional bloating, flatulence, belching, and distention are all considered normal parts of digestive physiology, especially after eating. These symptoms typically aren’t considered a problem until they begin to cause pain and/or disrupt your daily life.
Let’s take a look at some cases where this can occur.
Stress and Irritable Bowel Syndrome (IBS)
IBS is a common gut disorder and is a frequent cause of bloating and abdominal distention. One study found that all patients with diagnosed IBS, regardless of the subtype, experience more sensations of bloating than healthy controls. Furthermore, nearly half of IBS patients experienced physical abdominal distention [10].
The link between stress and IBS is well-researched, and chronic stress often increases IBS-related symptoms such as:
- Gas, bloating, and abdominal distention
- Constipation
- Diarrhea
- Stomach pain
- Cramping
Those with IBS tend to struggle with mental health disorders, and research shows that they experience higher levels of depression, anxiety, and distress than the general population [11]. Additionally, people with IBS tend to have higher levels of stress and a lower quality of life [12].Fortunately, IBS can be treated with functional medicine, offering some much-needed relief for IBS-related mood disturbances.
While we’re unsure of the exact mechanism by which stress increases symptoms of IBS, studies show that stressors alter the microbial balance and production of gut flora metabolites. This change in the microbiome then causes physiological changes in the brain via the gut-brain axis [13].
When the brain creates a stress response, chemical messengers—like stress hormones and neurotransmitters—travel down the gut-brain axis and can cause hypersensitivity in the gut. In fact, research shows that IBS patients may not actually experience more gas production than healthy populations. It’s likely a hypersensitivity reaction in the enteric nervous system that leads to increased sensations of bloating [14].
Regardless of the exact mechanism, there appears to be a strong correlation between IBS symptoms and stress.

Bloating in Other GI Conditions
Because of the communication between the digestive system and the brain, stress likely increases symptoms of bloating and abdominal distention in other functional GI disorders.
For example, as stress can cause dysbiosis in the digestive tract, it’s likely a major contributing factor in the development of small intestinal bacterial overgrowth (SIBO). Additionally, exocrine pancreatic insufficiency and histamine intolerance both frequently present with bloating, and are likely aggravated by chronic stress [15, 16].
Food intolerances and allergies commonly present with bloating and are another example of how stress affects the GI tract [17, 18]. For example, sensitivities like wheat and gluten intolerance are caused by a misguided immune reaction in the gut. As stress creates inflammation and an abnormal immune response in the digestive tract, it may also lead to the development and persistence of these sensitivities.
Other Possible Causes of Bloating
Many other chronic health conditions can often present with abdominal bloating and distention. This includes disorders and other underlying factors like:
- Certain medications
- Hypothyroidism [1, 2]
- Obesity [1]
- Type-2 diabetes [2]
- Autoimmunity [2, 19, 20]
- Menstruation and ovarian cysts [21, 22, 23]
Even musculoskeletal disorders are often triggered by stress and can cause increased bloating and abdominal distention. The following are two examples of when this may occur.
Abdominal Muscle Dysfunction
Abnormal contractions in the diaphragm and belly muscles after eating can cause the nervous system to create a heightened sense of bloating. This abnormal “viscerosomatic reflex” causes poor posture and distention of the abdominal muscles, and may worsen bloating sensations [24].
Exercises that retrain the muscles to contract in a normal way after eating may reduce the perception of bloating [24].
Pelvic Floor Dysfunction
Stressful situations naturally cause our muscles to tighten and can lead to increased contractions in the muscles of the pelvic floor. These muscles control our bladder, bowel, and sexual function. When they are overly contracted (too tight) they can create a condition known as high-tone pelvic floor dysfunction [25].
Conversely, the opposite can happen when the pelvic floor muscles become overly relaxed, making it difficult to have regular bowel movements. In either case, both increased tone and over-relaxation of these muscles can lead to a wide array of symptoms, including bloating [25].
It’s believed that people with pelvic floor dysfunction likely have disordered gut-brain connections [26]. Biofeedback is a mind-body therapy that teaches your body how to relax and can help restore the gut-brain axis. One clinical trial on women with pelvic floor dysfunction found that over half of the participants had decreased bloating after undergoing biofeedback [26].
This positive response further strengthens the evidence that our brains and digestive tracts are connected. Overall, stress appears to increase the likelihood of bloating by affecting multiple body systems, including the digestive, nervous, and musculoskeletal systems.

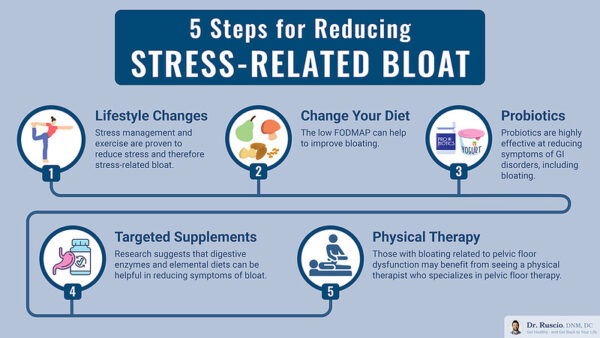
Your 5-Step Guide to Reducing Stress-Induced Bloating
While much of the following research on relieving stress and GI symptoms was performed on those with IBS, we’ve found the below therapies to be helpful for people with other conditions that result in bloating and abdominal distention.
Step 1: Lifestyle Changes
Stress management: Stress-reduction techniques can reduce the “fight or flight response” that happens during times of stress and can improve your gut health. Cognitive behavioral therapy (CBT), biofeedback, and meditation all help reduce stress levels and relieve stress-induced bloating [27, 28, 29].
One meditation technique in particular, mindfulness-based stress reduction (MBSR), shows promise in reducing bloating and overall stress levels. Additionally, results may last up to six months after undergoing MBSR therapy [30, 31, 32].
Gut-directed hypnotherapy may also significantly reduce symptoms of bloating, anxiety, and depression. These effects were seen in as few as six sessions [33, 34, 35].
Exercise: Physical activity is beneficial for improving stress, alleviating uncomfortable GI symptoms, and improving overall wellness. For the best results, aim to engage in moderate physical activity for two to three hours per week [36]. This includes activities like:
- Fast walking
- Biking on a flat surface
- Water aerobics
- Basketball, tennis, volleyball, and other sports
Yoga also appears to be an effective exercise for reducing bloating and is well-known to help reduce stress and anxiety levels [37].
Step 2: Change Your Diet
Start by following an elimination diet to help heal your gut, reduce inflammation, and determine which foods might be triggering your symptoms.
A good place to start is with a Paleo diet framework. The Paleo diet emphasizes high-protein, high-fat, and low-carbohydrate consumption. It reduces inflammation in the intestinal tract and can be effective at eliminating digestive symptoms, like bloating and distention. This is a well-rounded diet that eliminates several common triggers without being overly restrictive.
Common triggers that are eliminated on the Paleo diet include:
- Sugar
- Processed foods
- Gluten-containing foods and other grains
- Dairy
If, after trying it for two to three weeks, the Paleo diet doesn’t work for you, try switching to a low FODMAP diet. Clinical trials show that a low FODMAP diet is highly effective at reducing abdominal pain, gas, and bloating, while improving the overall quality of life [38, 39, 40, 41, 42].
Try the low FODMAP diet for two to three weeks and see if your symptoms improve. If they do, it may not be necessary to continue to follow a strict low FODMAP protocol to maintain relief from your symptoms, as 84 percent of participants in one study still experienced relief from their digestive symptoms, even after reintroducing a few FODMAP foods [43]. In fact, long-term restriction of FODMAP foods may actually worsen symptoms, as it suppresses the growth of healthy gut flora [44].
It is important to note that everyone’s food triggers may be different and it may take some experimentation to figure out what may be causing your bloating and other GI symptoms.
Once you eliminate all of the suspected triggers from your diet, you can start adding foods back in, one at a time. Introduce a new food every two to three days, and watch to see if you experience any bloating or distention. This will allow you to identify your unique gut triggers, without being overly restrictive.
Step 3: Introduce Probiotics
Probiotics are highly effective at reducing symptoms of GI disorders, including bloating and abdominal distention [45, 46, 47, 48]. Probiotics help to dampen the dysbiosis that occurs from stress and can help restore the normal gut flora.
In patients with IBS, probiotics can significantly reduce abdominal pain, and even help to alleviate bloating and diarrhea that accompany menstruation [48, 49, 50, 51].
It’s important to note that prebiotics, food-based supplements that promote the growth of beneficial gut bacteria, may not offer the same benefits [52].

Step 4: Targeted Supplement and Dietary Treatments
If your bloating and/or stomach distention isn’t solved by dietary and lifestyle changes alone, it may be time for a more targeted approach.
- Supplements: Research suggests that digestive enzymes can help reduce symptoms of bloating, abdominal pain, and flatulence [53, 54]. One enzyme in particular, ɑ-galactosidase, may be beneficial in alleviating colic in children and is considered to be safe [55].
- Intermittent Fasting: One study showed that intermittent fasting successfully reduced bloating, abdominal pain, diarrhea, nausea, and anxiety in those with IBS [56]. Intermittent fasting focuses on abstaining from eating for a certain period each day. Many people start with a 16-hour fasting window, but there are many variations, and you should always do what’s best for you.
- Elemental Diet: Don’t worry if fasting isn’t appropriate for you, as an elemental diet can effectively resolve stubborn IBS-related symptoms, like gas and bloating, in just two to three weeks [57]. The elemental diet is formulated to be easily digested, it reduces inflammation in the GI tract, and helps increase nutrient absorption. The elemental diet is easy to incorporate and can be used alone, or alongside another diet.
- Medications: Rifaxamin is a popular antibiotic that’s used to treat dysbiosis and infections in the GI tract. It’s considered safe by health care practitioners, as it’s not absorbed into the bloodstream, lessening its side effects. Rifaxamin is highly effective at reducing IBS symptoms, particularly bloating, and it may take as little as two weeks to see significant results [58]. Furthermore, rifaxamin may offer long-term relief from bloating, even after finishing the course of antibiotics [59].
Step 5: Physical Therapy
Those with bloating related to pelvic floor dysfunction may benefit from seeing a physical therapist who specializes in pelvic floor therapy. Manual physical therapy can effectively break up adhesions (scar tissue) that constrict organs and lead to abdominal distension and bloating sensations [60].
As previously discussed, pelvic floor biofeedback may help alleviate bloating, lessen constipation, and improve overall well-being [26].
Summary: Can Stress Cause Bloating?
Research supports that stress is a likely cause of bloating in both GI disorders and non-gut-related conditions. The gut-brain axis provides a powerful pathway of communication between the brain and digestive tract, allowing stress to increase inflammation and dysbiosis in the gut.
Fortunately, there are some basic steps that you can take to improve your symptoms of bloating and abdominal distention.
Stress reduction, dietary changes, probiotics, supplements, and even physical therapy are all likely effective in improving bloating.