With a slew of tools to trick out immune cells, researchers are expanding the repertoire of CAR-T therapies.
Crystal Mackall remembers her scepticism the first time she heard a talk about a way to engineer T cells to recognize and kill cancer. Sitting in the audience at a 1996 meeting in Germany, the paediatric oncologist turned to the person next to her and said: “No way. That’s too crazy.”
Today, things are different. “I’ve been humbled,” says Mackall, who now works at Stanford University in California developing such cells to treat brain tumours. The US Food and Drug Administration approved the first modified T cells, called chimeric antigen receptor (CAR)-T cells, to treat a form of leukaemia in 2017. The treatments have become game changers for several cancers. Five similar products have been approved, and more than 20,000 people have received them. A field once driven by a handful of dogged researchers now boasts hundreds of laboratory groups in academia and industry. More than 500 clinical trials are under way, and other approaches are gearing up to jump from lab to clinic as researchers race to refine T-cell designs and extend their capabilities. “This field is going to go way beyond cancer in the years to come,” Mackall predicts.CRISPR cancer trial success paves the way for personalized treatments
Advances in genome editing through processes such as CRISPR, and the ability to rewire cells through synthetic biology, have led to increasingly elaborate approaches for modifying and supercharging T cells for therapy. Such techniques are providing tools to counter some of the limitations of current CAR-T therapies, which are expensive to make, can have dangerous side effects, and have so far been successful only against blood cancers. “These techniques have expanded what we’re able to do with CAR strategies,” says Avery Posey, a cancer immunology researcher at the University of Pennsylvania in Philadelphia. “It will really take this type of technology forward.”
Even so, the challenge of making such a ‘living drug’ from a person’s cells extends beyond complicated designs. Safety and manufacturing problems remain to be addressed for many of the newest candidates. “There’s an explosion of very fancy things, and I think that’s great,” says immunologist Michel Sadelain at the Memorial Sloan Kettering Cancer Center in New York City. “But the complexity cannot always be brought as described into a clinical setting.”
Revved up and ready to go
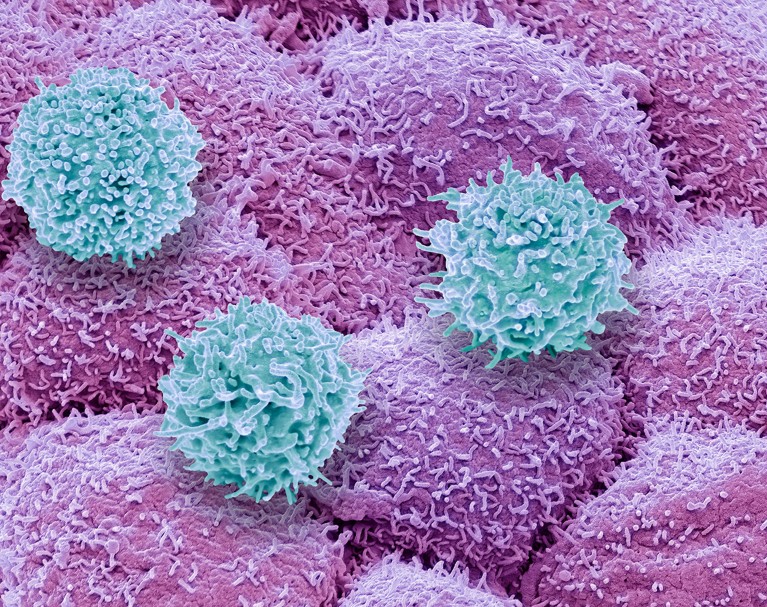
CAR-T therapies capitalize on the activities of T cells, the immune system’s natural hunters that prowl through the body looking for things that don’t belong. Foreign cells, or those infected with a virus, express unusual proteins that serve as a beacon to T cells, some of which release a toxic stew of molecules to destroy the abnormal cells. This search-and-destroy function can also target cancer cells for elimination, but tumours often have ways of disarming the immune system, such as by cloaking abnormal proteins or suppressing T-cell function.
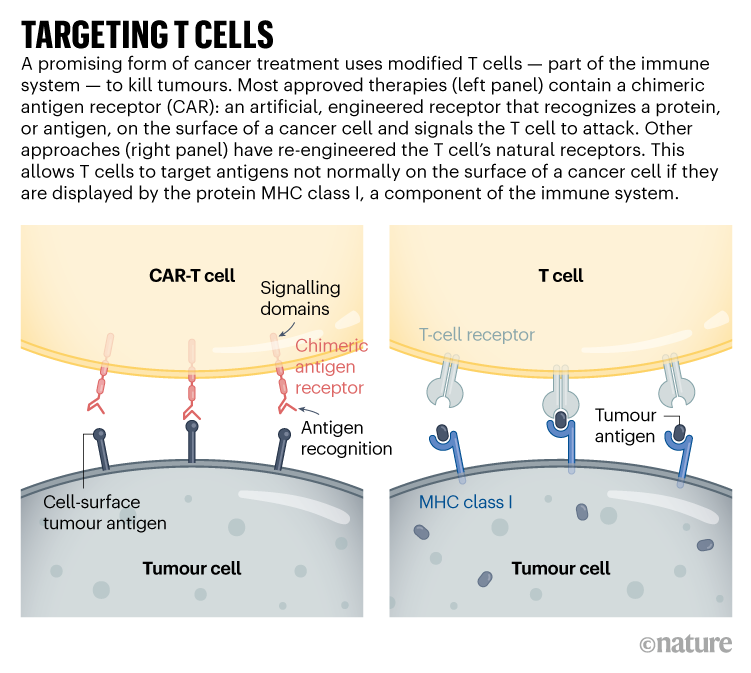
CAR-T cells carry synthetic proteins — the chimeric antigen receptors — that span the cell membrane. On the outside is a structure that functions like an antibody, binding to specific molecules on the surface of some cancer cells. Once that has bound, the portion of the protein inside the cell stimulates T-cell activity, hot-wiring it into action. The result is a tiny, revved-up, cancer-fighting machine.
Approved CAR-T therapies target one of two proteins found on immune cells called B cells, and are used to treat certain forms of leukaemia and lymphoma that involve the unchecked proliferation of these cells. The proteins — CD19 and BCMA — are not unique to cancer, meaning that the therapies kill B cells indiscriminately. However, people can live without these cells.
There is still plenty of room for improvement in CAR-T therapies. Although the effects can be long-lasting — sometimes even curative — cancer eventually returns in most people who have been treated. Solid tumours, such as those found in lung or pancreatic cancers, have so far not responded convincingly to CAR-T cells. The therapy has safety risks and can, in rare instances, be fatal. And it must be custom-made for each recipient, using their own T cells as a starting point, resulting in a relatively slow and expensive manufacturing process.
As yet, there are no simple solutions to any of these problems. “We clearly have a long way to go,” says Mackall. “But we’re now seeing promising signals.”
Some progress is being made against solid tumours. These often contain a heterogeneous mosaic of cells that have different combinations of mutations. This means that a CAR-T therapy directed at a particular mutated protein might work for only one subset of cells. The tight mass of a solid tumour can also be difficult for T cells to penetrate, and researchers have struggled to find suitable targets that won’t wreak havoc in healthy tissues.
Despite this, some clinical trials have shown glimmers of efficacy. Mackall and her colleagues have engineered CAR-T cells to target a molecule called GD2, which is expressed at high levels by some brain and spinal-cord cancers called gliomas. The team gave one intravenous dose of CAR-T therapy to people with gliomas, then administered multiple, lower doses directly into the brain. She and her colleagues reported last year that three of four people treated in this way responded positively1. “These cells just dive right into the brain,” says Mackall. “And the body doesn’t reject them up there — it’s playing in that immune-privileged space.”
Targeting solid tumours could require T-cell therapies that recognize more than one mutated protein or that can target cancer cells expressing higher levels of a given protein than normal cells do. One clinical trial that reported results in November 2022 took this to the extreme: rather than using CARs, the team used CRISPR to engineer natural T-cell receptors (see ‘Targeting T cells’) to recognize mutated proteins found in each participant’s tumour2. The individuals received a mixture of cells targeting different proteins, in the hope that solid tumours would be less likely to develop resistance to a therapy with multiple targets. Tumours stopped growing in 5 of the 16 participants 28 days after treatment. Researchers hope to tweak the protocol, including giving higher doses, to boost effectiveness.
The ability to track and fine-tune T-cell activity is also improving, says immunologist Carl June at the University of Pennsylvania. Through advanced single-cell analyses, researchers can follow the fate of both the engineered cells and the tumours they are designed to kill. They can determine which T cells have become ‘exhausted’ — a dysfunctional state that can come from prolonged stimulation — and which tumour cells are becoming resistant to treatment. They can also see whether the environment surrounding a CAR-T-treated tumour has become riddled with immune-suppressing cells (such as macrophages or regulatory T cells). Overcoming that local immune suppression will be key to harnessing T cells to fight solid tumours, says Yangbing Zhao, chief scientific officer at UTC Therapeutics, a biotechnology company headquartered in Singapore that is developing CAR-T therapies. “No matter how many targets you target, if the tumour is evading the immune response, it won’t work,” he says.
June and his colleagues used a single-cell approach to study resistance to CAR-T therapies that target CD19, and found that CAR-T products that were less able to activate certain helper T cells were associated with the emergence of resistance3. They also used single-cell techniques to learn more about why CAR-T cells directed against a protein called mesothelin, found in pancreatic cancer cells, often fail. Reducing the activity of two genes in CAR-T cells might bolster the therapy4. “We’re going to be able to understand these resistance mechanisms,” says June. “And then with all of these tools like CRISPR, we’re going to engineer around them.”
In addition to editing T cells, CRISPR has been used to find more ways of modifying them. Immunologist Alexander Marson at the Gladstone Institutes in San Francisco, California, and his colleagues used CRISPR to activate or suppress thousands of genes in T cells, and then looked at the effect the changes had on the production of crucial immune-regulating proteins called cytokines5. In another screen using CRISPR, the team found that reducing the activity of a protein called RASA2 enhanced the ability of CAR-T cells to kill their targets6. “We’re learning lessons about the genes that we can turn up and turn down to tune T cells to behave as we want,” says Marson.
Synthetic biologists have also set their sights on T cells, and are engineering sophisticated cellular circuits that could allow greater control over the expression of CARs and other proteins that might increase T-cell activity. In December last year, synthetic biologist Wendell Lim at the University of California, San Francisco, and his colleagues reported7 that they had engineered T cells to express both a CAR and IL-2, an immune-regulating protein. IL-2 can improve T-cell penetration into solid tumours and overcome the immunosuppressive signals that tumours release, but it can be toxic when administered systemically. Letting the T cells produce IL-2 enables local administration of the protein, which could bypass its toxicity to other tissues.Last-resort cancer therapy holds back disease for more than a decade
Other synthetic circuits have been designed to allow precise regulation of CAR expression, by placing it under the control of genetic elements that activate the necessary genes in response to a drug8. So far, however, most of these complicated designs have not yet gone through the safety studies and standardization required for use in people, says Sadelain.
Researchers are learning so many lessons that a big question for the field is now determining which engineered T cells to take forwards into human studies, says oncologist Marcela Maus at Massachusetts General Hospital in Boston. “We can invent and innovate so much in the lab, but there is this funnel of translating that into clinical trials,” she says. “There’s so many things we can do. We have to figure out which are the best things to tweak and test in trials.”
Costly business
Manufacturing CAR-T cells is already wildly complex by pharmaceutical standards. So far, all approved therapies require engineering a person’s own T cells to express the CAR. That adds to the time and thus the cost of producing the therapies: in the United States, a single treatment with CAR-T cells can be about US$500,000, not including the cost of hospitalization and associated treatments.
Creating CAR-T cells that can be given to multiple people — often called off-the-shelf cells — has long been viewed as crucial to lowering the price of the therapy. But early results suggest that there is still work to do, says bioengineer Rahul Purwar at the Indian Institute of Technology Bombay. Although the cells can be edited to reduce the chance that they will themselves be eliminated by the immune system, early trials suggest that they do not survive long after infusion and might still be rejected (see, for example, ref. 9)9. “Off-the-shelf is a great approach,” he says. “It is coming, but right now we are not yet there.”Cancer treatments boosted by immune-cell hacking
The therapy is also rarely available outside wealthy countries. In Brazil, haematologist Renato Luiz Guerino Cunha at Oncoclínicas Group in São Paulo was the first in the country to treat someone with CAR-T therapy in 2019. But progress has been slow, he says: he lacks the capacity to rapidly produce large quantities of cells. “In three years, we treated just six patients,” he says. “We need new technology for the processing.”
Producing a CAR-T cell therapy typically involves using a type of virus called a lentivirus as a vector to shuttle in the synthetic CAR gene. But more research into gene therapies has increased demand for clinical-grade lentiviruses. Researchers now wait months and pay top dollar to complete their experiments; Cunha produces his own but can do so only in tiny quantities. Improvements to CRISPR gene editing could help in this regard.
Despite the challenges, CAR-T therapies continue to expand, with some of the hundreds of clinical trials worldwide exploring entirely new applications. Last year, researchers reported promising results in a small trial of CAR-T therapies to treat a form of the autoimmune disease lupus10. And in a study in mice, researchers reprogrammed T cells without the usual first step of removing them from the body, creating CAR-T cells designed to clear scar tissue from the heart11.
In December, June and his colleagues unveiled a way to streamline cell production. At the American Society of Hematology’s annual meeting in New Orleans, Louisiana, the team announced12 that reducing manufacturing times and engineering CAR-T cells to express a protein called IL-18 boosted their efficacy and allowed researchers to reduce the dose of cells given to people. “Those patients had incredible responses,” says Maus of the clinical trial, “which gives you this really tantalizing hint that if you engineer the T cell better, you can make it even more powerful.”
Source: Nature