Day: 12/17/2022
Adeno-Associated Mediated Gene Transfer for Hemophilia B:8 Year Follow up and Impact of Removing “Empty Viral Particles” on Safety and Efficacy of Gene Transfer
Abstract

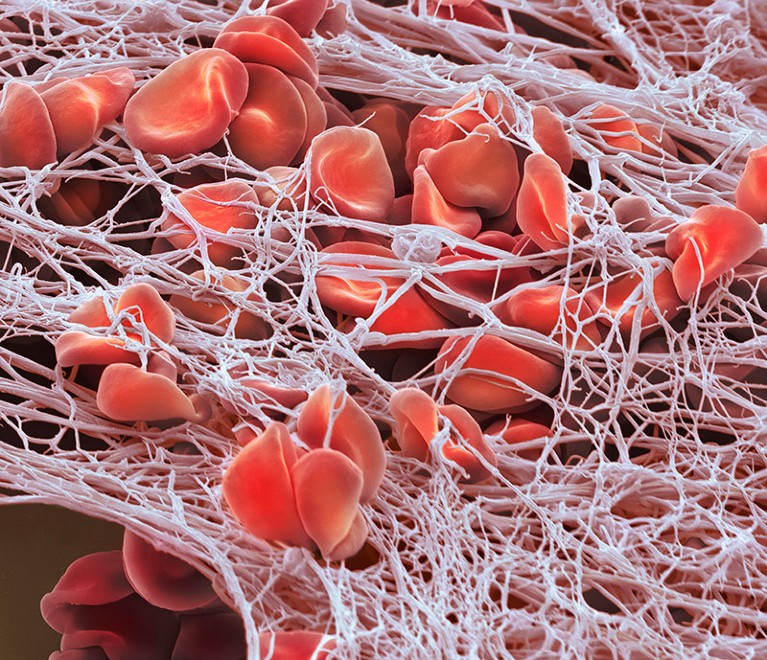
Background: We have previously shown that a single intravenous administration of a self-complementary adeno-associated virus (scAAV) vector containing a codon-optimised factor IX gene, under control of a synthetic liver specific promoter and pseudotyped with serotype 8 capsid, (scAAV2/8-LP1-hFIXco) resulted in a dose-dependent increase in plasma FIX levels in all 10 enrolled severe hemophilia B (HB) patients (ClinicalTrials.gov:NCT00979238; Nathwani et al 2011). FIX activity was stably maintained for at least 3 years (Nathwani et al 2014) but concerns over FIX expression declining over time remain. This is because AAV-mediated transgene expression is mediated mainly by episomally retained viral genomes, which may be lost with natural hepatocyte turn-over. The only vector-associated adverse event was an asymptomatic rise in liver enzymes associated with a decline in FIX levels, occurring within 3 months of gene transfer in two-thirds of the patients treated at a dose of 2×1012 vector genomes(vg)/kg. Liver enzymes normalized with corticosteroids without complete loss of transgene expression. There was no long-lasting toxicity over a period of 3 years but further follow-up is required. The vector preparation used contained an excess of empty capsids, which lacked a full-length viral genome, and are therefore, non-functional but capable of provoking an immune response against transduced hepatocytes. Therefore, a new clinical preparation of scAAV2/8-LP1-hFIXco was manufactured from which most of the empty particles were removed by caesium chloride density centrifugation in the hope that this would reduce the risk of hepatotoxicity. We report on the evaluation of this new vector preparation in severe HB patients and provide an update on up to 8 years follow-up of our original cohort of patients.
Methods: Ten subjects were recruited in 2010-2012 to the initial dose-escalation/extension study arm, which entailed a single intravenous infusion of scAAV2/8-LP1-hFIXco (full: empty capsid ratio ~1:10) at a dose of either 2×1011vg/kg, 6×1011vg/kg or 2×1012vg/kg. Two severe HB patients (FIX <1%) were enrolled into the first and mid-dose cohorts, with six patients treated at the high dose. In a follow-on study arm, two severe HB subjects received a dose of 2×1012vg/kg of the new scAAV2/8-LP1-hFIXco preparation (full: empty capsid ratio 1:3) whilst the next 2 patients were treated at a dose of 5×1012vg/kg. In both arms, vector was administered without prophylactic immunosuppression but corticosteroids (starting at 60mg/day) were commenced if liver enzymes increased to ≥2 fold over baseline levels after gene transfer.
Results: Transgenic FIX activity levels have remained stable in all 10 subjects treated in the initial dose escalation/extension arm over a median follow-up of 6.7±1.0 years with mean levels in the three dose cohorts at the time of reporting of 1.9±0.6, 2.3±0.3 and 5.1±1.4 IU/l respectively. Over this period, annual FIX concentrate usage has dropped by 66% and annual bleed rate has declined by 82% when compared to pre-gene therapy levels. No late toxicity was observed. Neutralising antibodies to FIX were not detected in any patient but anti-AAV8 capsid-specific antibody levels persisted at high titres in 9 of 10 patients. In patients treated with the new preparation of scAAV2/8-LP1-hFIXco (median follow up = 2.1±1.4 years), mean FIX activity in the 2×1012vg/kg dose cohort was 2.6±0.7 IU/l. This is lower than observed previously at this dose level, but the difference is not statistically significant. Mean steady state FIX levels in the 5×1012vg/kg cohort were 17±5 IU/l. FIX antigen to activity ratio was 1:1. Elevation of serum alanine aminotransferase was observed in 3 of 4 patients treated with the new vector preparation, requiring treatment with corticosteroids.
Conclusion: This is the first report to demonstrate stable therapeutic expression of FIX in patients with severe HB over a period of 8 years following systemic administration of scAAV2/8-LP1-hFIXco without late toxicities. We show for the first time that reducing the capsid load by removing empty AAV capsids does not appear to reduce the incidence of hepatotoxicity in patients with severe HB suggesting that other factors are involved in the aetiology of this process.
source:https://ashpublications.org
Researchers welcome $3.5-million haemophilia gene therapy — but questions remain
The world’s most expensive drug has the potential to save lives. But it cannot treat the most common form of the disease.
On 22 November, the US Food and Drug Administration (FDA) approved the first gene therapy for the genetic blood-clotting disorder haemophilia B — a one-time treatment that costs US$3.5 million.
Hemgenix — developed by the pharmaceutical company CSL Behring, based in King of Prussia, Pennsylvania — uses a modified virus to deliver a gene to the recipient’s liver cells. The gene codes for a protein involved in blood clotting called factor IX, which people with the disease are unable to produce.
Clinical trial data suggest that the single dose of Hemgenix will provide people with moderate to severe haemophilia with adequate protection from uncontrolled bleeding for eight years, and potentially longer.
But the treatment’s hefty price tag makes it the most expensive drug in the world. And although it seems to be effective, gene-replacement therapies for the most common form of haemophilia remain elusive.
Significant savings
CSL Behring says the cost is justified. In a statement, the company said that even at a cost of $3.5 million, Hemgenix could save the US health-care system $5 million to $5.8 million per person treated, because of its proven effectiveness at decreasing or eliminating the need for regular injections of factor IX. People with haemophilia B (who account for 15% of haemophilia cases) are currently given factor IX once or twice a week. The protein is required to form blood clots, but people with the disease lack the gene required to make it in sufficient quantities. If the condition is left untreated, people experience uncontrolled bleeding that can be life-threatening.CRISPR gene therapy shows promise against blood diseases
“Living with haemophilia is all about where one is born,” says Glenn Pierce, vice-president of the World Federation of Hemophilia in Montreal, Canada. “In the US, the treatment of an adult with haemophilia B averages $700,000–800,000 per year. The high price of Hemgenix will pay for itself in a relatively short time, and assuming it lasts.”
But scientists worry that the price would not be affordable in low- and middle-income countries, where most people with haemophilia live and where supplies of treatments and factor IX are often insufficient. “As new technologies such as gene therapy emerge on the scene, those who would benefit most can least afford to pay. We cannot leave the majority of the world behind,” says Pierce. CSL Behring declined to comment on the drug’s pricing beyond its public statement.
Promising results
The latest clinical trial of Hemgenix, which included 54 people with haemophilia B, reported a 54% reduction in the number of bleeding episodes per year, and 94% of participants discontinued any prophylactic therapy within two years of receiving the single dose. “The patients start making factor IX very quickly … in seven to eight months after the single dose, for nearly all patients, the level of factor IX had stabilized,” says Andrew Nash, CSL Behring’s chief scientific officer.
Even the lowest response in the clinical trial, a 10% increase in factor IX levels, is sufficient to prevent spontaneous bleeding, researchers say. But patients might require top-up prophylaxis treatments after injuries, or if they’re having major surgery and their factor IX levels are less than 50%.
“If you’re in the 10–40% range, you could still get a problem with major trauma or surgery. But you can pretty much forget about haemophilia,” says Edward Tuddenham, a consultant haematologist at University College London and part of the research group that designed the viral vector that CSL Behring licensed.Four Success Stories in Gene Therapy
Tuddenham and his colleagues showed in an eight-year follow-up study of a clinical trial of a similar drug for haemophilia B that there are good reasons to consider gene therapies a stable and durable treatment1.
“The approval of Hemgenix is a key milestone on the road to a cure, and it appears likely some recipients will indeed be cured for many years,” says Pierce.
Immunity issues
The FDA’s approval highlights difficulties in the quest to develop gene therapies for haemophilia more generally. Only 15% of people with haemophilia have haemophilia B. Most have haemophilia A — a genetic disorder caused by a deficiency in a different blood-clotting protein called factor VIII, which is encoded by a different gene.
Finding an effective gene therapy for haemophilia A has proved challenging, because a greater increase in factor VIII production is needed to get a good therapeutic effect, and some clinical trial participants have shown strong immune responses to the viral vector used to deliver the gene.
“In haemophilia A, there is an obvious waning off with time and [the gene expression] may only last for eight years,” says Michael Makris, who studies haemostasis and thrombosis at Sheffield University, UK. “Once you have adeno-associated viral gene therapy, you make antibodies to the AAV vector, so you cannot have it again.”
On 24 August, the European Medicine Agency approved a gene therapy for haemophilia A by BioMarin Pharmaceutical, based in San Rafael, California. After rejecting their first application, the FDA is now considering BioMarin’s resubmission.
“Gene therapy — while exciting and promising — should not be considered lightly,” says Leonard Valentino, a former haemotologist who is chief executive of the US National Hemophilia Foundation in New York City. “It is a potentially life-changing decision, and with any life-altering decision, there can be positive and negative effects”.
Nature 612, 388-389 (2022)
doi: https://doi.org/10.1038/d41586-022-04327-7
References
- Nathwani, A. C. et al. Blood 132 (S1), 491 (2018).
Source: Nature
Three ways to combat antimicrobial resistance
With a dearth of new antibiotics coming to market, researchers are finding creative ways to keep bacteria at bay.
The need to find new antibiotics is pressing, but many scientists and policy makers are tackling antimicrobial resistance from other angles. Nature Index takes a look at three methods in more detail.
A plasma wash
Plasma-activated water, enriched with chemically unstable versions of oxygen and nitrogen — also known as radical and reactive species — is being considered as potential new disinfectant. “If bacteria are overwhelmed with radicals then they end up dying,” says Katharina Richter, a biomedical researcher at the University of Adelaide in Australia.
Richter and her colleagues are studying how fast plasma-activated water can clear wounds infected with methicillin-resistant Staphylococcus aureus (MRSA) compared with wounds left untreated. They’re also comparing the technique against administering an antibiotic through an intravenous drip. She says the initial results, which are yet to be published, are encouraging. “The treatment improved the wound and cleared the infection faster than without treatment,” she says. It wasn’t as effective as treatment with antibiotics, but Richter says the experimental design could be to blame. “We compared it with IV antibiotics and that isn’t comparing apples with apples. It would be fairer to compare it to antibiotics given topically. Our next study will have better controls.”
Metallic marvel
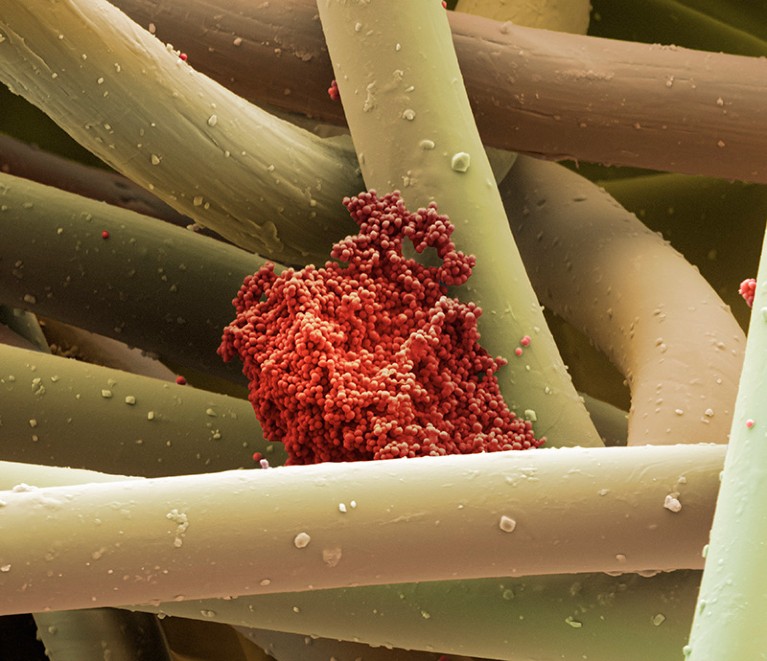
Bacteria, although single cells in nature, do get together and help each other to evade drugs and antiseptics. One way they do that is by forming biofilms — groups of bacteria living in a slimy milieu of their own making. Biofilms protect the individual cells residing within; it’s thought that roughly 80% of chronic human infections are caused by biofilms.Nature Index 2022 Biomedical sciences
The metallic element, gallium, interrupts bacteria’s uptake of iron, which eventually starves the microbes of nutrition. Because of this, gallium-laced drugs are one avenue being explored as a way to undermine biofilms. Scientists at the University of Manchester, UK, have found that gallium compounds can reduce the growth of bacteria by as much as 87% (J. M. Baker et al. Life Sci. 305, 120794; 2022). This work builds on the results of researchers at Shanghai Jiao Tong University in China showing that gallium can effectively dissolve the structure of MRSA biofilms, allowing the bacteria to be killed with one-tenth of the usual dose of an antibiotic (W. Xia et al. ACS Infect. Dis. 7, 2565–2582; 2021). Research is now focusing on how best to deliver the gallium and in what doses.
Molecular visas
An antibiotic should have three key characteristics: solubility; the capacity to readily bind to bacteria; and the ability to penetrate cell membranes. That makes designing a new antibiotic a tough task.
Instead of creating completely new antibiotics, therefore, some researchers are sifting through large digital libraries to predict which existing compounds might already have what it takes. “There are established methods for assessing the first two characteristics in a matter of minutes, but permeation is the missing piece of the puzzle,” says Javad Deylami, a computational chemist at the biotech start-up BIOptimize in Singapore.
That means that scientists are often assessing compounds that would theoretically be good at killing bacteria, but fall short at the first hurdle of getting inside the bacteria, says Deylami. “It’s like they reach a border but don’t have a visa to pass.”
Deylami has constructed a computerized version of the outer cell membrane of a bacterium on which he conducts simulations, testing the ability of molecules to penetrate the membranes. His model determines the forces affecting a would-be drug as it passes or fails, allowing Deylami to calculate the permeability of compounds.
Running known molecular structures through the program, Deylami’s team is able to learn, with the help of artificial intelligence, what qualities a compound needs to increase its permeability. That knowledge should help them to hunt through massive libraries to find existing drugs that have these properties.
Source: Nature
Tumor-Infiltrating Lymphocyte Therapy or Ipilimumab in Advanced Melanoma
Abstract
Background
Immune checkpoint inhibitors and targeted therapies have dramatically improved outcomes in patients with advanced melanoma, but approximately half these patients will not have a durable benefit. Phase 1–2 trials of adoptive cell therapy with tumor-infiltrating lymphocytes (TILs) have shown promising responses, but data from phase 3 trials are lacking to determine the role of TILs in treating advanced melanoma.
Methods

In this phase 3, multicenter, open-label trial, we randomly assigned patients with unresectable stage IIIC or IV melanoma in a 1:1 ratio to receive TIL or anti–cytotoxic T-lymphocyte antigen 4 therapy (ipilimumab at 3 mg per kilogram of body weight). Infusion of at least 5×109 TILs was preceded by nonmyeloablative, lymphodepleting chemotherapy (cyclophosphamide plus fludarabine) and followed by high-dose interleukin-2. The primary end point was progression-free survival.
Results
A total of 168 patients (86% with disease refractory to anti–programmed death 1 treatment) were assigned to receive TILs (84 patients) or ipilimumab (84 patients). In the intention-to-treat population, median progression-free survival was 7.2 months (95% confidence interval [CI], 4.2 to 13.1) in the TIL group and 3.1 months (95% CI, 3.0 to 4.3) in the ipilimumab group (hazard ratio for progression or death, 0.50; 95% CI, 0.35 to 0.72; P<0.001); 49% (95% CI, 38 to 60) and 21% (95% CI, 13 to 32) of the patients, respectively, had an objective response. Median overall survival was 25.8 months (95% CI, 18.2 to not reached) in the TIL group and 18.9 months (95% CI, 13.8 to 32.6) in the ipilimumab group. Treatment-related adverse events of grade 3 or higher occurred in all patients who received TILs and in 57% of those who received ipilimumab; in the TIL group, these events were mainly chemotherapy-related myelosuppression.
Conclusions
In patients with advanced melanoma, progression-free survival was significantly longer among those who received TIL therapy than among those who received ipilimumab.
Source: NEJM